Some Mental Health Issues More Common in MS Patients
HARTFORD, CT—Emotional disorders are common in patients with multiple sclerosis and can complicate treatment, according to the American Academy of Neurology.
The specialty group noted on its website that one-third to one-half of MS patients will have a major depressive episode in their lifetimes, compared to one-fifth in the general population. In addition, anxiety disorders affect more than one-third of MS patients, and adjustment disorders are diagnosed in nearly one-fourth.
Serious mental health issues, such as bipolar disorder occur in 13% of MS patients vs. less than 5% of those without the disease, and suicide is estimated to be twice as common in people with MS.
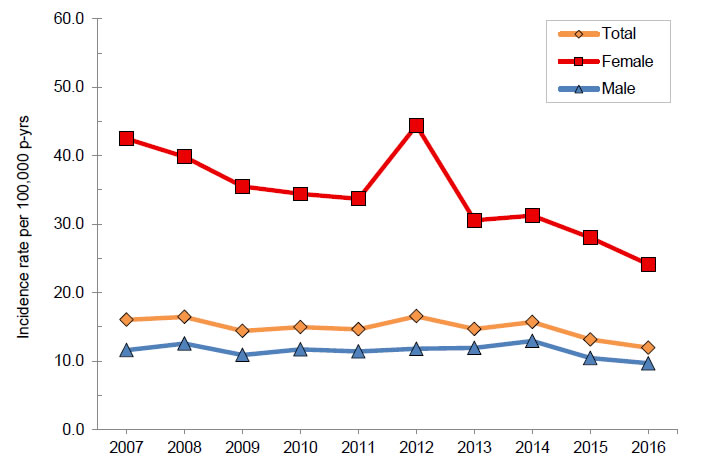
Annual incidence rates of multiple sclerosis, total and by sex, active component, U.S. Armed Forces, 2007–2016
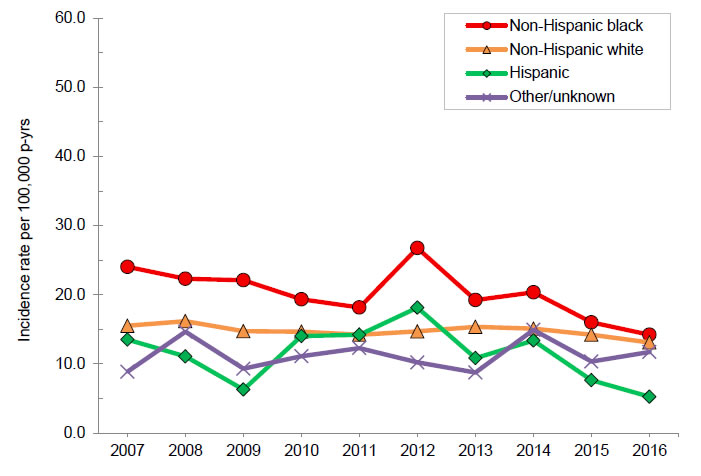
Annual incidence rates of multiple sclerosis, by race/ethnicity, active component, U.S. Armed Forces, 2007–2016.
Source: Multiple Sclerosis Among Service Members of the Active and Reserve Components of the U.S. Armed Forces and Among Other Beneficiaries of the Military Health System, 2007–2016. August 2017.Vol. 24 No. 8 MSMR.
Those effects might be further magnified in MS patients who have served in the U.S. military, where post-traumatic stress disorder, brain injuries and sleep problems can be co-morbidities, according to recent research.
“If persons with MS are struggling with cognitive, emotional and health-related behavioral issues, it is important that we identify these problems early and get them the care they need to manage them,” said Elizabeth S. Gromisch, PhD, a research neuropsychologist at the Mandell Center for Multiple Sclerosis at Mount Sinai Rehabilitation Hospital, Trinity Health Of New England, in Hartford, CT.
“For instance, if an individual has a neuropsychological assessment, not only can we identify what difficulties they are experiencing, but also their cognitive strengths, which can be used to help them work around their deficits,” she told U.S. Medicine.
Gromisch and her colleagues from the VA Connecticut Healthcare System in West Haven, Yale University and other New England institutions, recently published a study in Muscular Sclerosis & Related Disorders on the use of mental health services in veterans with MS.1
“As cognitive, emotional and health-related behavioral issues are common in persons with MS, screening for these issues are an important first step to identifying if there is a need for either neuropsychological or psychotherapeutic services,” Gromisch noted.
Until now, however, researchers and clinicians have not known “how many participate in neuropsychological and psychotherapeutic services and whether the presence of certain co-occurring conditions increase service use,” the study authors wrote.
The researchers sought to determine how often veterans with MS treated in the VHA system used neuropsychological and psychotherapeutic services and what factors affected utilization of those services. They looked at factors such as age, gender, education, race/ethnicity and co-occurring conditions.
Continue Reading this Article: Neuropsychological Services

