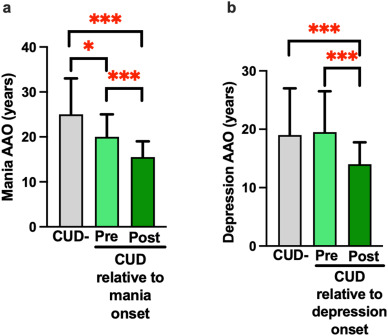
Click to Enlarge: Cannabis use onset pre-BD symptom age of onset (AAO) is associated with a later mood symptom AAO relative to cannabis use post-BD symptom AAO. a) Mania AAO was significantly earlier in the post-mania onset group (n = 14) compared to both the pre-onset group (n = 39); U = 105, p < 0.001) and CUD-group (U = 311.5, p < 0.001). Mania AAO was also significantly later in CUD-compared to pre-onset participants (U, 2268.5, p = 0.012). b) Post depression onset cannabis use (n = 24) was associated with significantly earlier depression AAO compared to CUD- (U = 988, p < 0.001) and pre-depression onset cannabis use (n = 28; U = 121, p < 0.001). Data represents median and interquartile range; ∗p < 0.05, ∗∗∗p < 0.001. Source: Journal of Psychiatric Research
SAN DIEGO — In bipolar disorder patients, having cannabis-use disorder and a natural tendency to go to sleep and awaken late are associated with more severe mood symptoms, according to a recent study.
The study published in the Journal of Psychiatric Research examined the relationship between chronotype, cannabis-use disorder and bipolar disorder mood symptoms. The authors investigated whether:
- Cannabis-use disorder was associated with bipolar disorder symptom onset,
- Initiating cannabis use impacts bipolar disorder symptom onset, and
- Chronotype, a substitute for circadian rhythm disturbance, was associated with bipolar disorder symptom onset.
They also explored whether cannabis-use disorder regulated the relationship between chronotype and bipolar disorder symptom onset.1
Bipolar disorder is a neuropsychiatric disorder with recurrent mood shifts between depressive and manic/hypomanic episodes that contribute to poor psychosocial and health outcomes, the researchers explained. Chronotype is an individual’s natural inclination to sleep and wake during a 24-hour period. Cannabis-use disorder is a condition that involves a problematic pattern of cannabis use that causes distress or impairs a person’s life, according to the Centers for Disease Control and Prevention (CDC).
The study authors are affiliated with the University of California, San Diego in San Diego and the VA San Diego Healthcare System in La Jolla, CA.
“Cannabis use is highly prevalent in people with bipolar disorder,” Alannah Miranda, PhD, a postdoctoral research scholar at the University of California San Diego, told U.S. Medicine. “Cannabis use has been associated with more severe bipolar disorder symptoms, however many people with bipolar disorder report using cannabis to help relieve symptoms associated with bipolar disorder. Our team wanted to help clarify the direction of the relationship between cannabis use and bipolar disorder by studying age of symptom onset and age of cannabis use onset.”
In this study, the investigators analyzed data collected from 212 patients with bipolar disorder type I, who participated in the Pharmacogenomics of Bipolar Disorder study. They assessed psychiatric and substance use disorders using the Diagnostic Interview for Genetic Studies and defined bipolar disorder diagnosis criteria using the Diagnostic and Statistical Manual of Mental Disorders IV.
The authors determined mood symptom age of onset, lifetime number of mood episodes and chronicity of cannabis using the Final Best Estimate method. They also calculated depression and mania episode density for each participant, which measures the number of mood episodes in a certain amount of time. Higher episode density corresponds to greater lifetime burden of mood episodes, according to the researchers.
Participants were divided into two groups: those with diagnosed cannabis abuse or dependence (n = 53) and those with no cannabis abuse or dependence (n = 159). Cannabis-use disorder patients were further separated into two groups: those who initiated cannabis use prior to or within the same year of mood symptom onset (pre-onset) and those who initiated cannabis use after mood symptom onset (post-onset).
In addition, participants were surveyed for chronotype using the Basic Language Morningness Scale, a 13-item composite self-report scale used to measure circadian rhythms. Higher summary scores indicated a higher level of morningness, the authors pointed out.
“Both evening chronotype (sleeping late/waking late) and cannabis use disorder were associated with more severe bipolar disorder mood symptoms, such as earlier age of bipolar disorder onset and more average mood episodes per year,” Miranda said. “However, people who began using cannabis before the onset of their mood symptoms experienced their first mood episodes later in life, compared to those who began using cannabis after their first mood episode. These findings indicate that cannabis use could be a form of self-medication of subclinical bipolar symptoms, or both cannabis use disorder and bipolar disorder share a common underlying mechanism, possibly related to sleep and circadian rhythm pathways.”
Circadian Rhythm Disruption
Study authors suggested the results offer possible evidence that circadian rhythm disruption could be an underlying factor that predisposes individuals toward both cannabis-use disorder and bipolar disorder.
For healthcare professionals who are treating patients with both bipolar disorder and cannabis-use disorder, Miranda recommends that cannabis use should be closely monitored and/or limited in people with bipolar disorder, given its association with worsening of mood and psychotic symptoms.
“Cannabis-use disorder is associated with worse bipolar symptoms, consistent with many other previous studies,” Miranda said. “More research is needed, however, because age of cannabis use onset and sleep patterns (chronotype) could potentially be used to identify onset of bipolar disorder or related psychiatric disorders.”
This study provides new evidence on the relationship between cannabis-use disorder, bipolar disorder and circadian rhythms. The authors propose that circadian rhythm disruption contributes to both cannabis-use disorder and bipolar disorder. They suggest that future studies could determine whether chronotype could be used as a biomarker to predict mood symptom onset in young adults at risk for developing bipolar disorder or identify patient groups at greater risk for developing cannabis-use disorder.
The researchers also pointed out this study is consistent with others that indicate circadian rhythm disruption could be a promising target for identifying cannabis-use disorder and bipolar disorder risk, and they recommend further studies to better understand the underlying neurobiology of this relationship and whether circadian rhythms can be leveraged to improve bipolar disorder and cannabis-use disorder outcomes.
The investigators acknowledged this paper has several limitations. The analyses didn’t include current depression and mania symptom data. Also, there was no limiting eligibility criteria for mood state for this study, and some patients presented with depression and mania/hypomania that could have impacted their memory, possibly affecting their ability to accurately recall the number of mood episodes.
Miranda noted that an upcoming study by the research team could offer more information about the link between cannabis use and bipolar disorder.
“Some of our team’s other research on cannabis use in people with bipolar disorder indicates that more moderate levels of use (i.e., weekly, but not daily) is associated with improvements in cognitive symptoms of bipolar disorder,” Miranda said. “These findings are soon to be published and could help our community better understand the relationship between cannabis use and bipolar disorder.”
- Miranda A, Holloway BM, Perry W, Minassian A, McCarthy M. Co-morbid cannabis use disorder and chronotype are associated with mood symptom onset in people with bipolar disorder. J Psychiatr Res. 2024 Dec;180:327-332. doi: 10.1016/j.jpsychires.2024.11.007. Epub 2024 Nov 4. PMID: 39515185; PMCID: PMC11646053.

