Seven Years Ago, Almost None Had Mandatory Vaccination
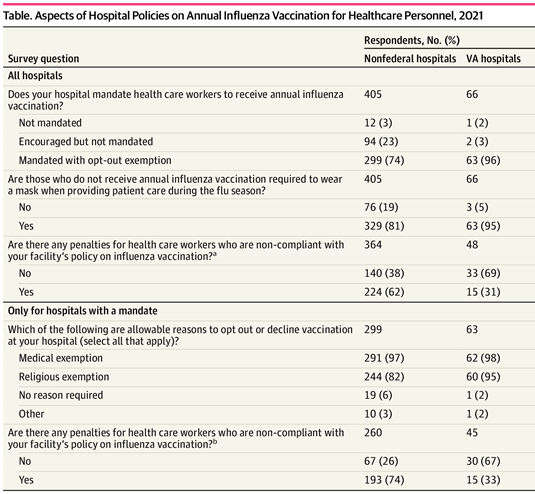
Click to Enlarge: Aspects of Hospital Policies on Annual Influenza Vaccination for Healthcare Personnel, 2021Abbreviation: VA, US Department of Veterans Affairs.
a. Fifty-one nonfederal infection preventionists (12%) responded with do not know or did not answer, and 18 VA infection preventionists (29%) responded with do not know.
b. Thirty-nine nonfederal infection preventionists (13%) responded with do not know or did not answer, and 18 VA infection preventionists (29%) responded with do not know. Source: JAMA Network Open
ANN ARBOR, MI — In 2017, almost no healthcare personnel at VA hospitals reported in a survey that they had received mandatory influenza vaccinations. By 2021, almost all VA respondents said they had.
A new research letter published in JAMA Network Open recently discussed what occurred at the VA compared to nonfederal hospitals.1
For years, the national Centers for Disease Control and Prevention (CDC) has recommended that all U.S. healthcare personnel (HCP) be vaccinated against influenza annually, but not all hospitals mandated it.
The Ann Arbor, MI, VA Healthcare System-led study pointed out that, in national surveys of hospitals in 2013 and 2017, influenza vaccination mandates increased from 44% to 69% in nonfederal hospitals but remained almost nonexistent—1% to 4% —in VA hospitals.
“We sought to ascertain how influenza vaccination requirements for HCP have changed since 2017, especially as mandatory HCP vaccinations were widely discussed during the COVID-19 pandemic,” the authors wrote.
The survey study is part of a multiyear, cross-sectional survey project that questions infection preventionists across the United States about health care-associated infection prevention practices.
The researchers in this study used the same national random sample as the 2017 survey wave. Beginning in April 2021, anonymous surveys were sent to 881 nonfederal general medical and surgical hospitals with intensive care units and all 127 VA hospitals. The survey responses were anonymous.
One of the questions was: Does your hospital mandate healthcare workers to receive annual influenza vaccination? Also assessed were declination or opt-out reasons, mask-wearing requirements and penalties for noncompliance, with analysis in January 2024.
The study team reported that the overall response rate was 48% (486 respondents from 1,008 nonfederal and VA hospitals in the sample). Of those, 15 respondents (10 from nonfederal and 5 from VA) did not answer the influenza vaccination mandate question and were excluded, leaving 471 respondents (405 from nonfederal and 66 from VA) for the analysis.
While nonfederal federal hospitals reporting mandatory influenza vaccinations for HCP rose slightly but not significantly, from 69% (365 of 526) in 2017 to 74% (299 of 405) in 2021 (P = 0.14), the increase was notable in VA hospitals. Mandatory influenza vaccines in VAMCs jumped from 4% (3 of 73) in 2017 to 96% (63 of 66) in 2021 (P < 0.001).
“Our findings show the impact of one of the largest healthcare systems in the United States taking a stand and putting a policy in place that is based in a bedrock ethical principle of medicine: Do no harm,” explained lead author Todd Greene, PhD, MPH, a VA patient safety researcher who also is affiliated with Michigan Medicine, the University of Michigan’s academic medical center. “In addition to the VA national directive, it is interesting to see how the COVID-19 era influenced flu vaccine requirements at non-VA hospitals.”
Nearly universal mandates at the VA followed the implementation of VHA directive 1192.01 in August 2020, which explicitly required VA HCP to either receive influenza vaccination or obtain an exemption annually as a condition of employment, the authors pointed out.
“The findings demonstrate that many hospitals have made institutional commitments to increase vaccination coverage among HCP through mandates,” the authors advised. “While mandates are a strategy to increase vaccination rates among HCP, they may not be wholly effective in the COVID-19 era. Recent data showed that vaccination rates among HCP, which were increasing before the COVID-19 pandemic (89% in 2017-2018 to 91% in 2019-2020), have steadily decreased during the pandemic (86% in 2020-2021 to 81% in 2022-2023). Common vaccine hesitancy issues (e.g., concerns about safety, mistrust of employers and authorities and violation of personal autonomy) may have affected this shift.”
The report also pointed out that nearly all VA and non-VA hospitals allowed for medical exemptions; 82% of non-VA and 95% of VA hospitals accepted exemptions for religious reasons. A very small minority of hospitals (6% of non-VA hospitals and 2% of VA hospitals) allowed waivers to be granted without a specific reason, the authors advised.
“There will always be vaccine hesitancy and concerns about bodily autonomy among health care workers, and seasonal flu vaccine effectiveness is variable,” Greene said in a U-M press release. “But for people working in the care environment, the benefits of getting vaccinated will generally outweigh any potential risks.”
The study was funded by the VHA National Center for Patient Safety.
- Greene MT, Linder KA, Fowler KE, Saint S. Influenza Vaccination Requirements for Health Care Personnel in US Hospitals. JAMA Network Open. 2024;7(6):e2416861. doi:10.1001/jamanetworkopen.2024.16861

