SAN FRANCISCO—The VA has successfully piloted a nationwide system to alert VA facilities when patients are admitted with a history of infection with two challenging multidrug resistant organisms (MDROs).
Details of the program, which is now in beta testing, were presented at ID Week 2018, held in San Francisco in early October.1
As the nation’s largest integrated healthcare system, the VA has long been a leader in addressing the development and spread of MDROs.
“Multi-drug resistant organisms cause infections that are very difficult to treat. This threat goes beyond the medical community. It is a public health crisis waiting to happen,” said Eli Perencevich, MD, MS, director of the Center for Comprehensive Access & Delivery Research and Evaluation (CADRE) at the Iowa City Veteran’s Affairs Health Care System. “The Veteran’s Health Administration is uniquely positioned to be a leader in this area and has the ability to make a real impact.”
The targeted organisms reflect the danger the spread of MDROs pose for healthcare systems. The U.S. Centers for Disease Control and Prevention (CDC) categorizes one of the organisms tracked by the alert system—carbapenem-resistant Enterobacteriaceae (CRE)—as an “urgent threat.”
Bacteria in this class “are immediate public health threats that require urgent an aggressive action.” CRE pose a particular threat to patients in medical facilities. The CDC reports that these highly resistant organisms can contribute to the death of up to 50% of those who become infected.
As of 2017, at least one species of CREs had been found in all 50 states and some cases of Enterobacteriaceae that have become resistant to all therapies or pan-resistant have been identified. The most common types of CRE seen in hospitals are carbapenem-resistant Klebsiella species and carbapenem-resistant E. coli. Both naturally occur in the human digestive system, but become dangerous when they spread elsewhere, particularly to the bloodstream. The multidrug resistant CREs have developed enzymes that break down carbapenems and other antibiotics, making them ineffective.
The CDC considers the other organism—methicillin-resistant Staphylococcus aureus (MRSA)—a “serious threat” that requires “prompt and sustained action to ensure the problem does not grow.” MRSA has been a focus of successful infection control efforts at the VA for several years. A MRSA Prevention Initiative introduced in late 2007 resulted in plummeting rates of MRSA infections in VA facilities. Over eight years, the program resulted in an 87% reduction in healthcare-acquired infections in VA intensive care units, an 80.9% drop in other units, an 80.9% decline in spinal cord injury units, and a 49.4% reduction in long-term care facilities.2
A central element of the MRSA Prevention Initiative involved screening patients for the organism at multiple points: admission, unit-to-unit transfer and discharge. The MDRO tracking and alert system brings additional, critical information to that surveillance process by tapping into the VA’s national database.
Piloted at 10 VA medical centers, the alert system continually monitors the VA Corporate Data Warehouse to identify new admissions anywhere in the nation of patients who have previously been identified as having CRE (ever) or MRSA (within the last year), explained Christopher Pfeiffer, MD, MHS, of the VA Portland Health Care System and the Oregon Health & Science University, both in Portland, Oregon, in his presentation at ID Week. When the system finds a match, it sends an alert to the infection prevention team at the admitting facility within four hours of the patient’s admission.
The pilot operated in the VAMCs in Portland, OR; Salt Lake City, UT; Iowa City, IA; Birmingham, AL; Boston; Madison, WI; Nashville; Bronx, NY; Pittsburgh and Lexington, KY. Researchers in each of the facilities as well as the VA’s National Infectious Diseases Services took part in the study.
Adopting the System
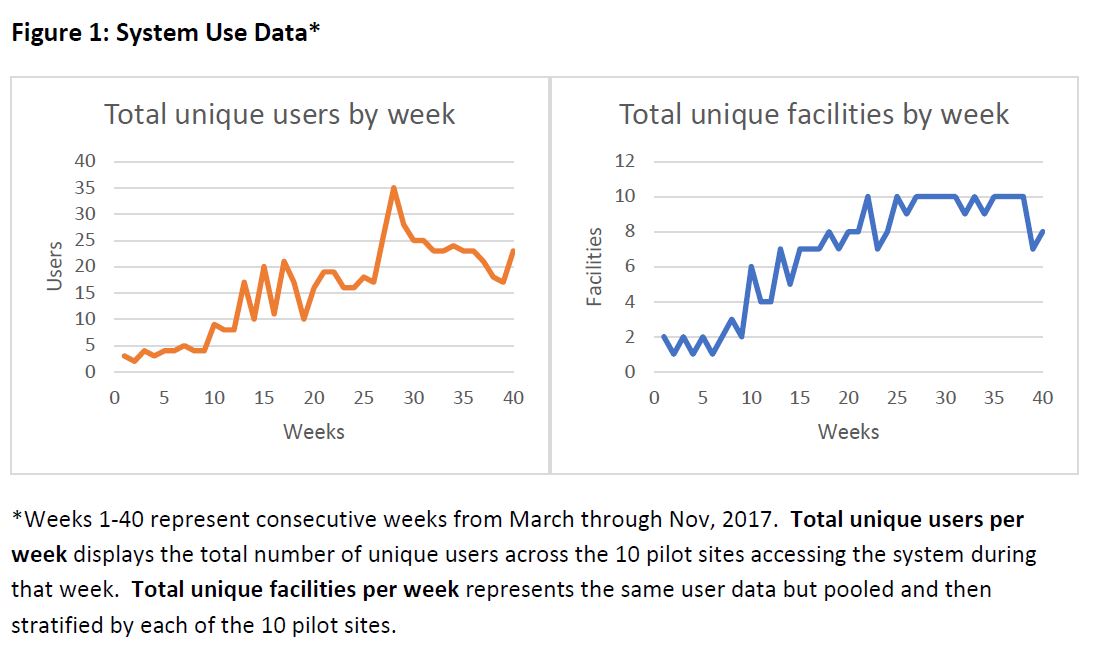
Infection prevention personnel at VAMCs took a while to adopt the system, but, after about seven months, the system had 35 unique users at its peak and 25 on a regular basis. All 10 facilities regularly used the tracking system within five months.
Adoption rose when Pfeiffer and his colleagues changed the formatting of the notifications to improve readability and reduced the time lag between admission to notification to a three to four-hour maximum.
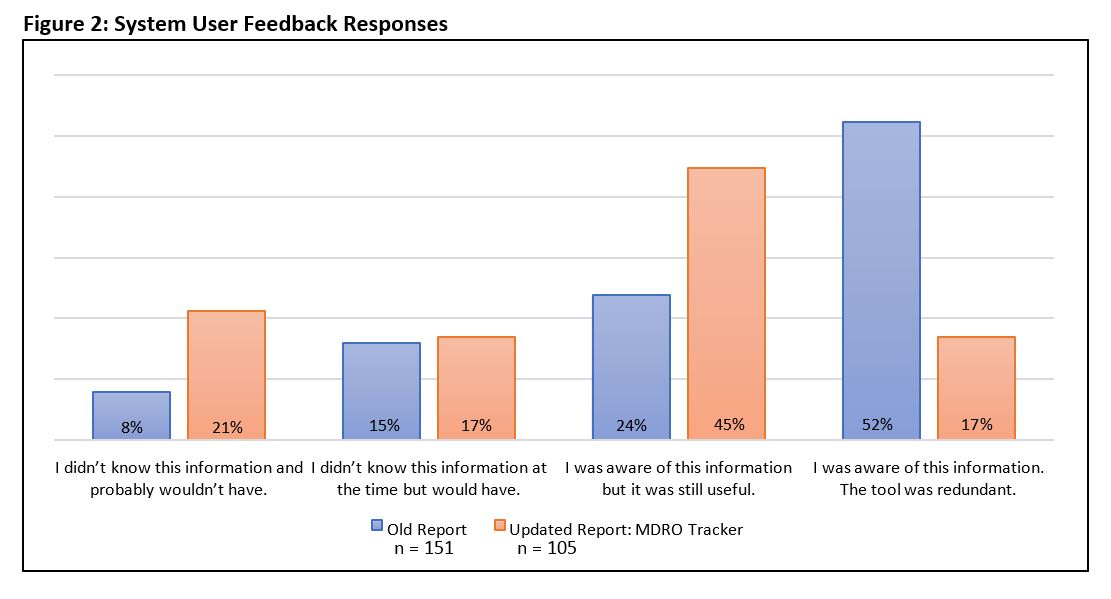
After the changes, one in five users said that the system gave them information they didn’t know and would not have discovered elsewhere compared to less than one in 10 before the upgrade. A total of 38% of users said the notification gave them new information. Just under half (45%) of the users found the information conveyed useful, even if they might have been aware of it, up from 24% before the changes. Only 17% found the updated alert system information redundant, down two-thirds from the 51% who provided feedback on the original version of the alerts.
The system provided significant value, according to the researchers’ analysis. During the study, 101 patients were identified with CRE. Of those, 11% had positive results from a different VA facility that triggered a notification. Among the 2390 patients with MRSA admitted during the study period, 214 or 9% were first flagged by the system with recent positive results at another VA facility. The researchers noted that these “results [were] unlikely to be known locally.”
The researchers also tested a convenience sample of CRE and MRSA patients to validate the system’s accuracy and determine whether the system would identify the MDRO before local staff. They found that the system flagged 21% of the 61 CRE patients and 71 of 1720 MRSA patients first.
Based on the results, Pfeiffer and his colleagues determined that the pilot demonstrated that a “novel automated MDRO alert system shows feasibility and potential for substantial utility” to assist in minimizing the spread of these organisms.
Such a program may prove to be a central element in combatting drug-resistant bacteria. As Perencevich said in announcing the VA’s research agenda for MDROs earlier this year, “Sustained, coordinated, and aggressive efforts to better understand and implement prevention strategies may help to evolve the current crisis into a more manageable problem.”
1. Pfeiffer C, Jones M, Klutts JS, Lee RA, Williams HB, West KA, Strymish JM, Safdar N, Harris BD, Gelman MA, Decker BK, Murray A, Aguilar N, Evans M. Pilot Implementation of a Nationwide Automated Multidrug-Resistant Organism Tracking and Alert Systemin Veterans Affairs. Poster Abstract Session 2161. ID Week 2018. October 6, 2018.
2. Evans ME, Kralovic SM, Simbartl LA, Jain R, Roselle GA. Eight years of decreased methicillin-resistant Staphylococcus aureus health care-associated infections associated with a Veterans Affairs prevention initiative. Am J Infect Control. 2017 Jan 1;45(1):13-16.


