 CHAPEL HILL, NC — The explosive emergence in December 2019 of a novel coronavirus in Wuhan, China, prompted governments around the globe to restrict travel from the affected region in an attempt to limit international spread of the disease. While these efforts focused on civilian mobility, they echoed concerns increasingly raised by military infectious disease specialists on the role of servicemembers as pathogen transmitters.
CHAPEL HILL, NC — The explosive emergence in December 2019 of a novel coronavirus in Wuhan, China, prompted governments around the globe to restrict travel from the affected region in an attempt to limit international spread of the disease. While these efforts focused on civilian mobility, they echoed concerns increasingly raised by military infectious disease specialists on the role of servicemembers as pathogen transmitters.
War and disease have always gone hand-in-hand; more combatants died from illness than injury in every significant conflict until World War I.1 For servicemembers, the expanded use of military forces to respond to international natural disasters, humanitarian crises, border control and epidemics pose another risk of exposure to pathogens.
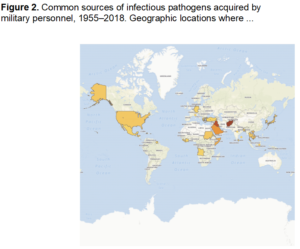
A recent article in The Journal of Infectious Diseases explored that risk, finding thousands of instances where military personnel transported active infections across borders during noncombat operations. As a result, they cautioned that deployments in response to societal disruptions create a “double-edged sword of mitigating one problem while creating another [that] may not be considered when decisions are made to deploy young, immunologically naïve [service members] to areas far from their homes.”2
As a former Navy infectious disease epidemiologist, “I knew that soldiers, sailors, airmen, and marines are at risk of such infections and sometimes share pathogens from deployment with others,” said corresponding author Gregory Gray, MD, MPH, professor, Division of Infectious Diseases, Global Health Institute and Nicholas School of the Environment at Duke University in Chapel Hill, NC. “However, never before had such a review been performed, and we found quite a few reports demonstrating the problems is a very important one to consider.”
In addition to facing a high risk for acquiring novel infectious diseases, servicemembers may also “inadvertently become carriers of pathogens, causing infections among close contacts within their military units or among community members at home or abroad,” Gray and his colleagues discovered in their analysis of 67 articles that documented instances of these transmissions between 1955 and 2018.
While advances in hygiene, mandatory immunizations and predeployment screening have dramatically reduced the impact of disease on servicemembers and their potential for pathogen transmission, these methods still fail with some regularity.
Notable Cases
In perhaps the most significant case, Nepalese peacekeepers, all of whom had passed a predeployment screening and none of whom were symptomatic for infection, imported Vibrio cholerae into Haiti in 2010. The resulting cholera outbreak sickened nearly 700,000 people and killed 8,500 by 2011, leaving behind an endemic disease that has subsequently affected at least 27,000 people per year.3
Similarly, American military personnel imported pandemic influenza A(H1N1) into Kuwait in 2009 with consequences beyond the spread of illness. “The introduction of the virus into Kuwait raised significant geopolitical concerns early in the pandemic when the severity of A(H1N1) pdm09 was still unclear,” noted Margaret Farrell, MD, now a senior program officer with the World Health Organization, and her former colleagues in an analysis of the outbreak investigation they conducted with the U.S. Global Disease Detection and Response Program, Naval Medical Research Unit No. 3, based in Cairo, and local Army medical units.4
That analysis found that the methods used to screen troops were insufficiently sensitive, particularly given the unknown virulence of the influenza strain at the time. The screening identified only 16% of A(H1N1) pdm209-positive servicemembers, while more than 91% of those isolated based on screening criteria turned out not to have the virus. Ultimately, movement of units carried pandemic influenza into Afghanistan and Iraq as well.
The spread of influenza in this instance and many others documented in the study came as no surprise to Gray. The pathogens of greatest risk for transmission include “rapidly transmittable respiratory viruses like influenza A viruses, novel coronaviruses (SARS, MERS, 2019-nCoV), adenoviruses and enteroviruses,” he told U.S. Medicine.
Co-author Jose L. Sanchez, MD, MPH, deputy chief, Armed Forces Health Surveillance Branch of the Defense Health Agency’s Public Health Division, added that “other pathogens such as enteric bacteria (diarrhea-causing) and enteric viruses as well as malaria are known to cause significant morbidity among U.S. military personnel deployed overseas and are also of significance.”
Malaria has plagued humans and military forces for millennia, with recent studies indicating that at least 1.5 million soldiers contracted the disease during World War I, facilitated by “transcontinental passages of parasites and human reservoirs of infection.”6 The return of infected troops brought the disease home and resulted in major epidemics with significant local transmission in England and Italy.
In recent decades, hundreds of U.S. and Jordanian servicemembers contracted the Plasmodium parasite during peacekeeping missions in Africa and other regions with endemic malaria, Gray and his colleagues found. While the U.S. Centers for Disease Control and Prevention reports intermittent small outbreaks of locally transmitted cases of malaria, the original sources are not clear. Jordan has no documented cases of secondary transmission, but it remains a risk as it also hosts competent vectors.5
Minimizing Risk
Gray and Sanchez recommended attending to the basics of infectious disease control to minimize the risk of disease transmission by servicemembers.
First, “commanders need to be made aware of health risks to their troops so they can enforce preventive countermeasures,” Sanchez told U.S. Medicine.
Then, all personnel should “follow the advice and guidelines of preventive medicine personnel,” Gray added. “If they tell you to receive a vaccine, take prophylactic medicine or render some other preventive advice, it is wise for you and others to follow.”
It is particularly important for deploying personnel to have preventive medicine consultations to reduce transmission and importation of multidrug resistant organisms, Gray said.
“Host nation personnel often have at least partial immunity from living where the pathogens are endemic or enzootic,” he noted, which explains why returning American servicemembers have higher rates of MDROs than are seen in the areas where they have been deployed. Thousands of instances of multidrug resistant infections have been found in recently returned servicemembers, with Acinetobacter species and Pseudomonas aeruginosa among the most common. While no secondary transmission have been reported, Gray said he and his fellow authors expect that those transmissions have likely been unreported or undetected rather than absent.
Sanchez urged servicemembers to “avoid the insect vectors by following personal preventive measures (such as skin and clothing repellent), avoid high-risk environmental conditions, if possible, and lower risk of enteric infections by avoiding high-risk and unapproved food sources that increase the risk of such pathogen infections.”
- Pennington H. The impact of infectious disease in war time: a look back at WWI. Future Microbiol. 2019 Feb;14(3):165-168.
- Zemke JN, Sanchez JL, Pang J, Gray GC. The Double-Edged Sword of Military Response to Societal Disruptions: A Systematic Review of the Evidence for Military Personnel as Pathogen Transmitters. J Infect Dis. 2019 Dec 15;220(12):1873-1884.
- Guillaume Y, Ternier R, Vissieres K, Casseus A, Chery MJ, Ivers LC. Responding to Cholera in Haiti: Implications for the National Plan to Eliminate Cholera by 2022. J Infect Dis. 2018 Nov 15;218(Suppl 3):S167-170.
- Farrell M, Sebeny P, Klena JD, Demattos C, Pimentel G, Turner M, Joseph A, Espiritu J, Zumwalt J, Dueger E. Influenza risk management: lessons learned from an A(H1N1) pdm09 outbreak investigation in an operational military setting. PLoS One. 2013 Jul 10;8(7):e68639.
- Jamain HM, Abu Shaqra QA, Kanani KA. Epidemiological pattern of imported malaria in Jordan from 2007 to 2011. Trop Biomed. 2013 Dec;30(4):591-5.
- Brabin BJ. Malaria’s contribution to World War One—the unexpected adversary. Mal J. 2014 Dec 16;13:497.

