Christine Hsu MD, Staff Clinician and Assistant Research Physician in the Liver Diseases Branch of the NIDDK
BETHESDA, MD — The risk of developing hepatocellular carcinoma, the most common type of liver cancer, is low for veterans who spontaneously clear hepatitis C virus (HCV) infection. It remains beneficial, however, to assess patients for other chronic liver diseases and related advanced fibrosis or cirrhosis, which are risk factors for liver cancer, according to a recent review article.
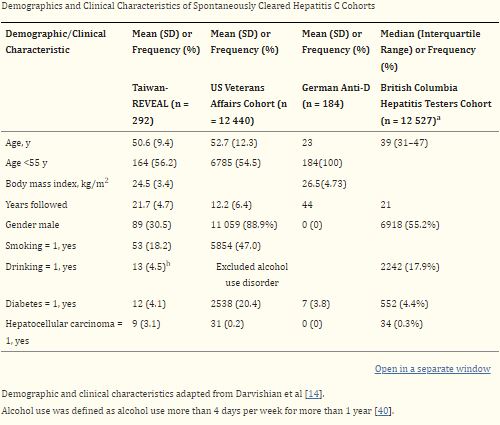
In the article published in Clinical Infectious Diseases, the researchers completed a systematic review of the literature and included 22 studies, primarily focused on patients with chronic hepatitis C who were cured and did not have cirrhosis, per the inclusion criteria. Because few studies reported the risk of hepatocellular carcinoma (HCC) after spontaneous HCV clearance, the study authors pointed out they also had collaborators from Taiwan, Germany and the VA to find three cohorts of patients who spontaneously cleared hepatitis C.1
The purpose of assessing HCC risk in spontaneously cleared HCV patients is to understand whether there are any long-term hepatocellular carcinoma risks of short-term hepatitis C infections in otherwise healthy individuals, the authors explained.
To try to capture the long-term hepatocellular carcinoma risk of a transient HCV infection, the researchers “estimated hepatocellular carcinoma risk in spontaneously cleared HCV and also in non-cirrhosis hepatitis C patients who are cured,” the article reported. A majority of the patients who spontaneously clear the hepatitis C infection (without treatment), will clear within the first six months of infection, the study authors explained.
The research team, which included authors from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) in Bethesda, MD, and the Corporal Michael J. Crescenz VAMC in Philadelphia, defined spontaneously cleared HCV as “positive hepatitis C antibody, but RNA negative without treatment.” For the patients who spontaneously cleared HCV infection, the article reported those who were HCV antibody-positive but HCV RNA-negative at diagnosis were included from three cohorts.
In the Risk Evaluation of Viral Load Elevation and Associated Liver Disease/Cancer-Hepatitis C Virus (REVEAL-HCV) cohort in Taiwan, patients from seven townships were invited to participate in a health interview and examination with blood collection. For this cohort, patients who tested positive for HCV antibody or hepatitis B surface antigen were followed with ultrasound and laboratory tests from 1991 to 2015. The German anti-D cohort is a cohort of women who had received HCV-contaminated anti-D immunoglobulin, which was given to Rh-negative women to avoid Rhesus isoimmunization from 1978 to 1979. The cohort of VA patients included U.S. patients who were found to be HCV antibody-positive but HCV RNA-negative at the initial diagnosis between 1999 and 2022.A
The authors explained they “decided not to combine their hepatocellular carcinoma risk as the three cohorts are very different.”
“We discovered the hepatocellular carcinoma (liver cancer) risk of those who spontaneously cleared their hepatitis C (HCV) to be very low and almost negligible,” lead author Christine Hsu MD, a staff clinician and assistant research physician in the Liver Diseases Branch of the NIDDK, told U.S. Medicine. “It was difficult to precisely estimate the risk using various cohorts of spontaneously cleared hepatitis C patients.”
The study’s most important finding is that, “even people with spontaneously cleared hepatitis C may still have other risk factors for hepatocellular carcinoma,” Hsu said.
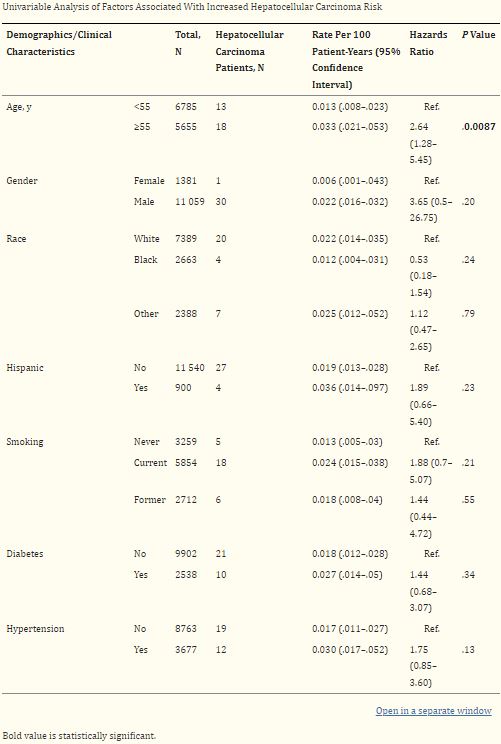
“People who have spontaneously cleared hepatitis C should be risk stratified for concomitant liver disease and consider calculating a FIB-4 (which is a non-invasive biomarker of fibrosis) because we discovered that even in these patients, Hispanic ethnicity, elevated liver enzymes, and high FIB-4 are risks for hepatocellular carcinoma development,” she emphasized.
Most of the hepatocellular carcinomas in hepatitis C are “discovered in patients with advanced fibrosis or cirrhosis, but occasionally patients without advanced fibrosis/cirrhosis can develop hepatocellular carcinoma. In large cohorts of patients with chronic hepatitis C who were treated and cured, risk factors for persistent hepatocellular carcinoma risk include chronic alcohol use and advanced fibrosis or cirrhosis,” according to Hsu.
Concomitant Liver Disease
“In people with spontaneously cleared hepatitis C (hepatitis C antibody-positive but hepatitis C RNA negative), it could be helpful to assess for concomitant liver disease such as Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) or at-risk alcohol use,” she advised. “Healthcare professionals could also consider using non-invasive biomarkers of fibrosis, such as FIB-4, to risk stratify for chronic liver disease, a risk factor for hepatocellular carcinoma.”
The results are significant, because “people who spontaneously clear their hepatitis C often don’t see a hepatologist or are even discharged from hepatology practice,” Hsu pointed out, adding, “It is thought people who spontaneously clear hepatitis C have little to no risk for hepatocellular carcinoma development absent of other risk factors. It is important to acknowledge that hepatocellular carcinoma risk may not be zero because of other potential liver-related risk factors, and those with certain liver-related risk factors should be followed regularly.”
The analysis determined that, in the VA cohort, the risk is 0.02 per 100 patient-years, while the risk of the German anti-D cohort (healthy pregnant women who incidentally received HCV-contaminated immunoglobulin before hepatitis C virus was discovered) was 0 in 44-year follow-up. While the REVEAL-HCV cohort in Taiwan was slightly higher at 0.14 per 100 patient-years, Hsu noted that hepatitis B “is endemic to Taiwan and past hepatitis B exposures were not clear in this cohort.”
“Past hepatitis B exposure is a contributory risk to developing liver cancer. Even with the VA cohort, many of the patients were tested for HCV because of risk factors and thus can confound outcome,” she said.
“Overall, the risk of hepatocellular carcinoma in patients who are transiently infected is very low and almost negligible. For people who had chronic hepatitis C who were cured and did not have cirrhosis, the overall risk is 0.33 per 100 person-years, which is also low,” Hsu advised.
A subanalysis of the VA cohort, which was the largest cohort of the spontaneously cleared hepatitis C patients in the article’s dataset, “showed that the Hispanic population and increased age (>55 years old) are at increased risk of hepatocellular carcinoma development compared to other ethnicities and younger patients,” she added.
“We speculate this may be related to underdiagnosed Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD),” Hsu said. “We discovered this even after excluding patients with defined definitions of MASLD. We will be presenting this data in an abstract at the American Association for Study of Liver Disease (AASLD) Annual Liver meeting this year.”
- Hsu CC, Gopalakrishna H, Mironova M, Lee MH, Chen CJ, Yang HI, Wiese M, Chang KM, Wright EC, Abijo T, Feld JJ, Kaplan DE. Risk of Hepatocellular Carcinoma After Spontaneous Clearance of Hepatitis C Virus and in Noncirrhosis Chronic Hepatitis C Patients With Sustained Virological Response: A Systematic Review. Clin Infect Dis. 2023 Aug 14;77(Suppl 3):S245-S256. doi: 10.1093/cid/ciad380. PMID: 37579210; PMCID: PMC10425144.