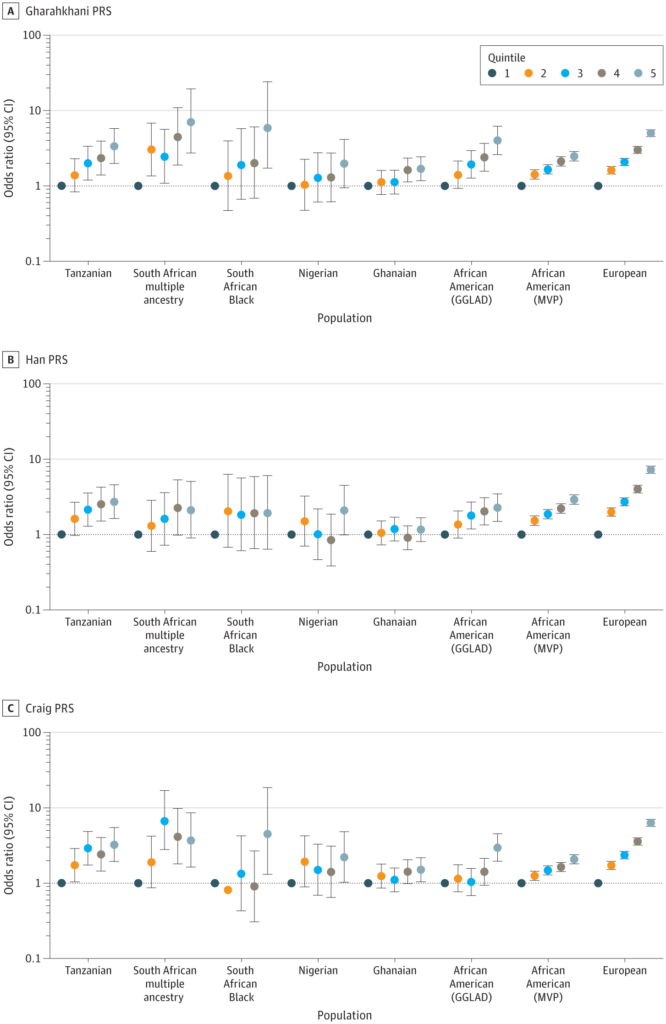
Odds Ratios by QuintileThe odds ratios (log scale) of risk for primary open-angle glaucoma from logistic regression by quintile for each of 8 study groups are displayed using 3 polygenic risk score (PRS) types: Gharahkhani PRS (A), Han PRS (B), and Craig PRS (C). Odds ratios (on a log scale) and 95% CIs are presented, allowing for comparison of risk across quintiles within each risk score type. GGLAD indicates Genetics of Glaucoma in People of African Descent; MVP, Million Veteran Program. Source: JAMA Network
CLEVELAND — Primary open-angle glaucoma (POAG), the most common type of glaucoma, develops gradually and is often asymptomatic in its early stages. Individuals of African descent face a prevalence of POAG that is 4–5 times higher than those of European descent, with the disease typically occurring earlier and progressing more aggressively in this population.
Despite these significant disparities, polygenic risk scores (PRSs)—which evaluate genetic risk by analyzing multiple DNA variants to identify individuals at higher risk for earlier or more tailored care—are still largely developed and validated using data from European populations, according to a new study.
“This gap in applicability limits clinicians’ ability to use PRSs effectively for these patients,” explained Neal Peachey, PhD, associate chief of staff for research at the VA Northeast Ohio Health System in Cleveland and an author of a new study that highlights the limitations of existing PRSs while demonstrating the urgent need for inclusive genetic tools.
The study, published in JAMA Ophthalmology, drew participants from three datasets: Genetics in Glaucoma Patients of African Descent (GIGA), Genetics of Glaucoma in Individuals of African Descent (GGLAD) and the Million Veteran Program (MVP). These datasets included individuals of African descent from Tanzania, South Africa, Ghana, Nigeria and the United States, as well as individuals of European descent from the United States.1
The researchers evaluated three PRSs developed using genomewide association studies (GWAS) on primarily European and Asian populations, Peachey said.
PRS performance was assessed using standard metrics relevant to clinical risk prediction, such as:
- Odds ratios (ORs): Comparing glaucoma risk between individuals in the highest versus lowest genetic risk categories.
- Area under the receiver operating characteristic curve (AUROC): Measuring overall predictive accuracy.
- Liability-scale R²: Estimating how much of the variance in glaucoma risk the PRS explained.
“The study yielded several important findings regarding the performance of PRSs for primary open-angle glaucoma in African ancestry populations compared to European ancestry populations,” Peachey told U.S. Medicine.
Among the findings:
- PRS performance was limited in African ancestry populations. The scores modestly predicted glaucoma risk in these groups but were significantly less effective compared to European ancestry groups.
- Results were better in admixed populations. African Americans and South African individuals with mixed ancestry showed slightly better PRS performance, likely due to their genetic similarity to populations used to develop the scores.
- Ancestry-specific factors matter. African ancestry populations have greater genetic diversity and unique patterns of linkage disequilibrium (LD), which likely reduce the effectiveness of PRSs developed for other groups.
- Inclusive research is needed. The findings emphasize the importance of conducting GWAS in African populations to create more representative and effective PRSs, which would support more equitable risk stratification and treatment planning.
“Overall, the results emphasize the need to develop and validate PRSs tailored for African ancestry groups to improve clinical risk stratification and promote equitable health outcomes,” Peachey explained. “Current tools, while moderately effective, are inadequate for accurately predicting glaucoma risk in these underserved populations.”
The principal investigator on VA funding for the study, he said the MVP Million Veteran Program (MVP)—the nation’s largest biorepository of veteran data—played a crucial role in this study by providing a large, diverse resource of genetic and clinical data, particularly for African Americans and European Americans. “MVP data not only enhanced the study’s scale and diversity but also underscored the disparities in the predictive performance of existing PRSs between African and European ancestry populations.” Peachey said. “This reinforced the need for more inclusive genomic research to develop equitable predictive models.”
The study serves as an important step toward closing gaps in genetic risk prediction for glaucoma in African ancestry populations, he advised. “By identifying where current tools fall short, it sets the stage for more inclusive research and equitable clinical tools. For clinicians, this represents progress toward ensuring that advances in precision medicine are accessible and effective for all patient populations.”
“Clinicians should recognize the limitations of current PRSs for primary open-angle glaucoma, especially for African ancestry populations,” Peachey continued. “Until more accurate, inclusive PRSs are available, clinicians should rely on traditional screening practices and remain vigilant in monitoring high-risk patients. Supporting and engaging in diverse genetic research can help bridge these gaps and improve care for all veterans.”
- Chang-Wolf JM, Kinzy TG, Driessen SJ, Cruz LA, et al. Genetics in Glaucoma Patients of African Descent (GIGA) Study GroupGenetics of Glaucoma in People of African Descent (GGLAD) Study GroupMillion Veteran Program (MVP). Performance of Polygenic Risk Scores for Primary Open-Angle Glaucoma in Populations of African Descent. JAMA Ophthalmol. 2024 Nov 14:e244784. doi: 10.1001/jamaophthalmol.2024.4784. Epub ahead of print. PMID: 39541127; PMCID: PMC11565374.

