Will Surgery Work?
The results comes with a strong caution, however. Fundoplication, anti-reflux surgery, creates a barrier to reflux of all gastric material—acidic and nonacidic—and, therefore, should relieve PPI-refractory heartburn that is reflux-related, according to the study.
“In practice, however, patients with “GERD symptoms” that are unresponsive to PPIs often do not have a response to surgery either,” the authors emphasized. “This might result from preoperative failure to document that the symptoms are truly reflux-related. Alternatively, for patients with reflux hypersensitivity, surgical reduction of reflux might not relieve symptoms generated by a hypersensitive esophagus.”
The authors called for systematic evaluation of patients, including esophageal MII-pH monitoring, which can distinguish PPI-refractory patients with non-GERD disorders, who will not benefit from fundoplication, from other patients with persistently abnormal acid reflux or reflux hypersensitivity, who have a chance for a positive response to surgery.
“MII-pH monitoring is a relatively recent innovation, however, and experts disagree on its clinical usefulness,” researchers pointed out, adding, “Surgeons are reluctant to rely on it to select patients for fundoplication, generally preferring traditional esophageal pH monitoring for that purpose. We hypothesized that, if non-GERD and functional disorders were excluded by systematic workup, then anti-reflux surgery would be superior to medical therapy for patients with PPI-unresponsive heartburn that MII-pH monitoring identifies as being reflux-related.”
The study described how five major mechanisms appear to underlie PPI-refractory heartburn:
- Abnormal acid reflux persists despite PPI therapy;
- The presence of reflux hypersensitivity, in which esophageal exposure to acid is normal but “physiologic” reflux episodes (acidic or nonacidic) evoke heartburn;
- That heartburn is caused by esophageal disorders other than GERD (e.g., achalasia);
- That heartburn is caused by extraesophageal disorders (e.g., heart disease); or
- That, heartburn is functional (i.e., not due to GERD or any other identifiable histopathologic, motility, or structural abnormality).
The issue remains, however, that therapy options are limited for patients with PPI-refractory heartburn that is reflux-related, due to persistently abnormal acid reflux or reflux hypersensitivity.
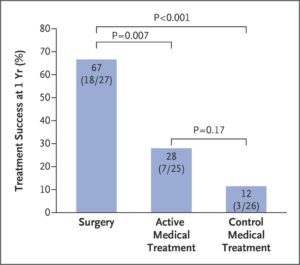
Treatment Success at 1 Year (Intention-to-Treat Analyses). Treatment success was defined as an improvement (decrease) of 50% or more in the GERD-HRQL score from baseline.
“PPIs are often continued despite inadequate symptom relief,” the authors wrote. “Other options include reflux-reducing medications, such as baclofen, or neuromodulators (e.g., tricyclic antidepressants) that dampen visceral hypersensitivity. However, baclofen and neuromodulators often have unacceptable side effects, and studies of their efficacy for PPI-refractory heartburn are few and of short duration. Recommendations for medical management of this condition are largely opinion-based.”
In an accompanying commentary, Nicholas J. Talley, MD, PhD, of the, University of Newcastle, Hunter Medical Research Institute, New Lambton Heights in Australia, wrote, “Conceptualizing gastroesophageal reflux disease (GERD) as a single disease process that will respond to higher and higher doses of acid suppression is a mistake. The underlying mechanisms that can lead to reflux of stomach contents into the esophagus and subsequent symptoms or esophagitis are probably diverse and contribute in varying combinations.”2
While Talley suggested placebo effect could have accounted for some of the positive surgery results, he also noted that persistent long term relief gave him confidence in the findings. Yet, few options remain if symptoms persist after surgery, he added, writing, “Unfortunately, we still have little to offer patients who despite a complete workup have troublesome reflux after surgery (as occurred in one-third of surgical patients in this trial), aside from repeat esophageal testing and yet another trial of acid suppression. There are no well-established endoscopic alternatives to surgery for acid-related heartburn, although research continues. Even though behavioral therapy approaches that involve techniques such as diaphragmatic breathing may be of value, clinical trials are few and not definitive. We need personalized medical options that target the underlying causes of GERD.”
- Spechler SJ, Hunter JG, Jones KM, Lee R, et. Al. Randomized Trial of Medical versus Surgical Treatment for Refractory Heartburn. N Engl J Med. 2019 Oct 17;381(16):1513-1523. doi: 10.1056/NEJMoa1811424. PubMed PMID: 31618539.
- Talley NJ. Think First, Cut Last – Lessons from a Clinical Trial of RefractoryHeartburn. N Engl J Med. 2019 Oct 17;381(16):1580-1582. doi:10.1056/NEJMe1911623. PubMed PMID: 31618545.

