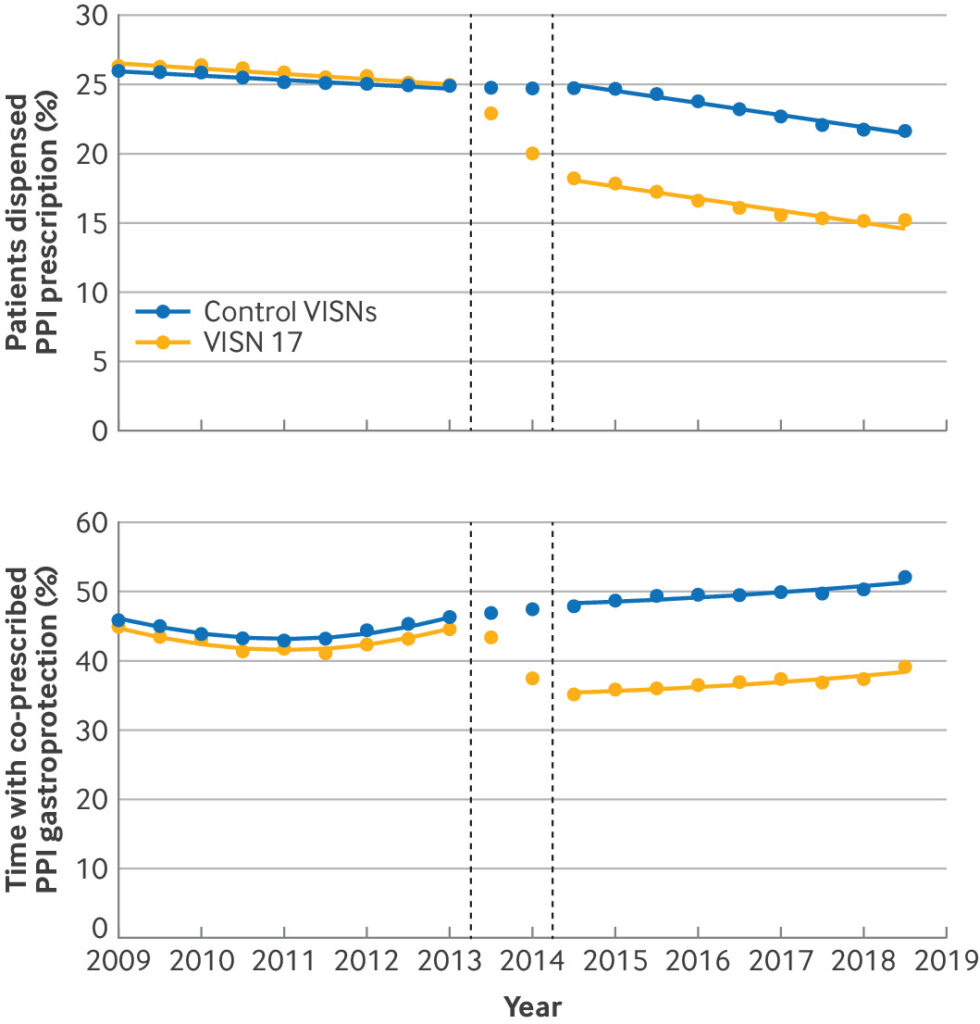
Click to Enlarge: Percentage of patients receiving proton pump inhibitor (PPI) prescriptions (top) and percentage of time with co-prescribed PPI in patients appropriate for gastroprotection (bottom) per 6 month period before and after implementation for Veterans Integrated Service Network 17 (VISN 17) and all other Veterans Affairs (VA) sites (controls), with fitted lines showing predicted percentages based on difference-in-difference regression models. For both outcomes, fitted lines were generated using predicted values for each time interval and site using difference-in-difference regression models after exclusion of data from 1 year implementation period (2013-14). Table 2 shows significant absolute changes associated with VISN 17 intervention in two outcomes based on models and their 95% confidence intervals, which exclude zero. Predictors included time (centered at implementation period), post-implementation period indicator, VISN 17 indicator (intervention), and interaction of VISN 17 by post-implementation. Robust standard errors were used to account for heteroscedasticity. For top panel, patients were included in numerator if they had received any PPI prescription dispensed by VA health system. Denominator included all patients who had ≥2 primary care visits during 2 years before interval. For bottom panel, patients were considered appropriate for gastroprotection during time that they had medication possession of ≥2 antithrombotic drugs with at least daily dosing (including anticoagulants, aspirin, and P2Y12 inhibitors) or an antithrombotic drug together with a non-steroidal anti-inflammatory drug with at least daily dosing. Patients were considered to have gastroprotection during time in which they had medication possession of a PPI with at least daily dosing. Only medications dispensed by VA were included.
ANN ARBOR, MI — One of the most commonly prescribed classes of drugs, proton pump inhibitors (PPIs), reduces the risk of gastrointestinal bleeding in certain patients at increased risk. Most PPI prescriptions are written for other reasons, however. In fact, an estimated 25-70% of PPI users might not have an appropriate indication.
This, along with research associating the use of PPIs with a number of medical conditions, has led to efforts to de-prescribe or reduce PPI prescriptions.
A new VA study, analyzing one of the largest of these efforts, sheds light on the promises and challenges of such an initiative while suggesting that certain concerns regarding PPI risk might be overestimated.
The deprescribing initiative was conducted in VISN 17 and imposed limits on PPI prescription size and refills for patients without a documented reason to be on the medication, discontinued old prescriptions and provided education to patients and clinicians on alternatives.
Funded by a VA grant to Loren Laine, MD, Sameer D Saini, MD, MS, and Yu-Xiao Yang, MD, MSCE, the study used electronic VA and Medicare data to examine the outcomes for patients in VISN 17 compared to patients in all other VISNs, who served as the control group, said the study’s first author, Jacob Kurlander, MD, MS. Using a statistical technique called difference-in-difference analysis—which involved examining trends before and after the intervention and comparing them to controls—the researchers were able to draw some conclusions about the effect of the intervention, explained Kurlander, a research scientist at the VA Center for Clinical Management Research in Ann Arbor, MI, and assistant professor in the division of gastroenterology at the University of Michigan.
The results were published recently in The BMJ.1
One finding was that the initiative resulted in a significant reduction in PPI prescriptions, the researchers reported in the British Medical Journal. At the start of the study, about 26% of veterans throughout the 18 regions who received primary care from a VA provider were prescribed a PPI in a 6-month period. By the end of the study period in 2019, only about 15% of veterans in VISN 17 had a PPI prescription, compared with about 22% of those in the other regions.
“Patients in VISN 17 had almost a 30% relative reduction in the percentage receiving PPIs, which is one of the strongest interventions that’s been done to reduce overuse of proton pump inhibitors,” Kurlander said.
Among the subset of patients at high risk of upper gastrointestinal bleeding, the use of PPIs went down by an absolute 11.3%—which was an unintended and undesirable consequence, he said.
Among the other findings of the analysis, there were no increases in primary care visits for upper GI diagnoses like nausea, heartburn or dyspepsia and no increase in endoscopies or hospital admissions for GI bleeding in older patients who were at high risk. And when the researchers looked at clinical conditions that had been associated with PPI use—kidney disease, fractures, pneumonia and cardiovascular disease—there was no reduction in any of the conditions with the exception of a very small (0.018%) reduction in the incidence of hip fracture—a reduction that was not clinically significant, but was statistically significant due to the large sample size, Kurlander said.
PPIs Not as Harmful?
“If PPIs were really a cause of a lot of harm, we would expect to see larger reductions in these conditions that have been associated with PPIs, so this provides some reassurance that PPIs are likely not as harmful as they are often thought to be,” he added.
In light of the study’s findings, Kurlander said the main benefits of a PPI describing intervention are likely to be a reduced pill burden for patients and economic benefits both for patients—who will have fewer copays—and the health system.
“Even though these medications are generic and not very expensive, because they are used often, the bill really adds up,” Kurlander said. In a separate analysis not included in this study, Kurlander and his colleagues estimated the cost savings of this initiative, if implemented system-wide, would be $328 million over 4½ years.
For now, he says the most important message for prescribers is to understand patients’ risk factors for bleeding—including medicines like aspirin, nonsteroidal anti-inflammatory drugs and anticoagulants, as well as the effects of age and history of GI bleeding—and think carefully about why a patient might be prescribed PPIs before discontinuing one.
Similarly, he says, when prescribing a new medication there has to be a good rationale for doing so. Ironically, he says many people who are recommended to take PPIs for prevention of upper GI bleeding do not receive them.
In short, Kurlander said, efforts to deprescribe must be balanced with efforts to prescribe appropriately. “When we focus too much on the overstated harms of PPIs, patients can miss out on the real benefits of these medications in preventing gastrointestinal bleeding.”
- Kurlander, J. E., Laine, L., Kim, H. M., Roberts, C. B., et al. (2024). Impact of large scale, multicomponent intervention to reduce proton pump inhibitor overuse in integrated healthcare system: difference-in-difference study. BMJ (Clinical research ed.), 385, e076484. https://doi.org/10.1136/bmj-2023-076484


