Other Important VA Studies at the American Diabetes Association 79th Scientific Sessions
MIAMI—The first-line drug of choice for Type 2 diabetes, metformin has long been known to effectively reduce blood glucose levels and substantially cut the risk of cardiovascular disease. It may also protect elderly diabetics from frailty, based on a study presented at the American Diabetes Association 79th Scientific Sessions last month by researchers at the Miami VA Healthcare System.
Frailty, a physiological decline in late life that increases vulnerability to stressors such as illness, trauma or loss, is associated with overall functional decline as well as significantly elevated risk of illness and mortality as well as increased use of healthcare services.
Diabetes accelerates aging and increases the risk of frailty through several mechanisms, according to study co-author Jorge G. Ruiz, MD, associate director for education and evaluation at the Miami VA Healthcare System Geriatric Research Education and Clinical Center and associate professor of clinical medicine at the University of Miami Miller School of Medicine.
“The most prominent mechanism for the association of frailty for diabetics is persistent low-grade inflammation. The catabolic effects of cytokines in muscle contributes to sarcopenia, a prominent feature of frailty, and systemic inflammation could affect many other systems in the body,” Ruiz told U.S. Medicine.
One of the underpinnings of T2D also plays a role. “Insulin resistance is another mechanism that can lead to frailty,” said study co-author Hermes Florez, MD, PhD, director of GRECC and professor of public health sciences and medicine at the University of Miami Miller School of Medicine.
In contrast, metformin use is associated with a “modest reduction in weight and inflammatory biomarkers, as well as improved cognition and mobility, and other studies have shown a reduction in the incidence and mortality associated with cancer,” Florez told U.S. Medicine.
To assess the impact of metformin on elderly veterans with diabetes, the researchers identified veterans over age 65 with T2D who also met the definition of frailty as determined by a 44-item frailty index. The retrospective study used data from the VA electronic health system to track the veterans’ health status and medication use. Patients were identified between January 2016 and August 2017 and followed through October 2018.
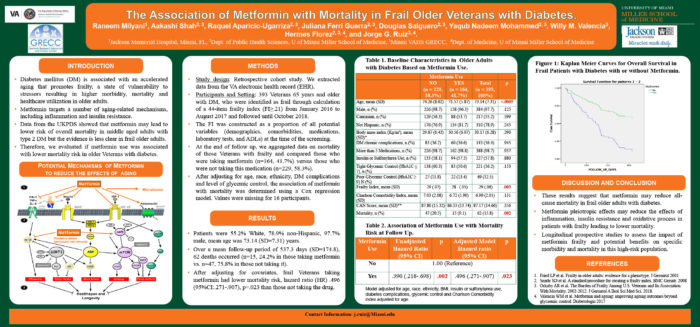
Of the 393 veterans who met the study criteria, 164 (41.7%) took metformin and 229 (58.3%) did not. While many veterans took more than one medication for diabetes, 23.6% did not take any medication for their diabetes.
Patients had an average age of 73.14 years, 97.7% were male, and 55.2% were white.
With a mean follow-up of 537.3 days, 62 veterans died. Of those, just 15, or 24.2%, were in the metformin group. On an unadjusted basis, metformin reduced the risk of death by 61%. After adjusting for covariates, the researchers found that frail veterans who took metformin had half the mortality risk compared to those not taking the drug.
“It appears metformin is a geroprotector at a molecular level,” Ruiz said.
That realization may take a while to spread into practice. “Years back, it was recommended that, if a patient had chronic heart failure, they should stop metformin because of the effect on kidney function. It turns out, metformin is beneficial for survival,” Ruiz noted.
“This subsample doesn’t necessarily represent the whole population of veterans. All of them were frail,” Florez noted. “But broadly, it’s important to know that metformin can be beneficial in veterans with multiple comorbidities unless absolutely contraindicated. It should be the first line for diabetics.”
“This is another piece of evidence reinforcing metformin for diabetes and for those who in the past have been denied the medication,” echoed Ruiz. “The findings are compatible with other evidence that metformin may benefit patients with frailty or prefrailty. Do not deny the drug; make every effort to keep patients on it.”
Researchers at the San Antonio VA are evaluating metformin in veterans with prefrailty, but the benefits of the 50 year old drug may extend even beyond diabetics, Ruiz noted. “Researchers with the National Institute of Health and other organizations are studying whether adults without diabetes may benefit from metformin’s geroprotective effects, such as improved cognition and physical function.”
Other VA Presentations at ADA
A team from the VA Central Iowa discussed an intervention to increase awareness and treatment of prediabetes that increased diagnosis rates sixfold. The Prediabetes Identification Dashboard and Treatment Plan Tool developed for the program identified 7,299 veterans who received care at the VA Central Iowa at high risk for prediabetes and diabetes with at least one HbA1c of between 5.7% and 6.4%. At the start of the intervention, only 17 veterans had the ICD-10 code for prediabetes in their health records. The dashboard helps primary care providers determine whether referrals for nutrition counseling, diabetes education, weight loss clinic, metformin or weight loss medication had been made and utilized. The ability to track recommendations and education was particularly important, as 97% of veterans identified during the program’s pilot preferred to receive education in primary care.
Another group of VA researchers found that predictive models for atherosclerotic cardiovascular disease that used pooled cohort equation variables developed by the American College of Cardiologists and American Heart Association along with VA-specific coefficients provided better discrimination that the pooled cohort equations or RECODe risk equations. Predictive power was further improved by adding hemoglobin A1c, estimated glomerular filtration rate, diabetes medications and statin therapy. They concluded that “health system-specific tailoring of prediction equations provides improved discrimination and calibration compared to existing models.” 3
Researchers at the Albany, NY, VAMC presented a study on the increase in blood lactic acid in elderly diabetic veterans with Stage 3 chronic kidney disease associated with metformin use. Metformin has recently gained U.S. Food and Drug Administration approval for use in this population. Higher levels of lactic acid and one case of mild lactic acidosis associated with higher doses of metformin led the team to recommend lower doses of metformin in elderly diabetic men with Stage 3 chronic kidney disease. 4
Other VA studies looked at the impact of psychosocial factors and nutrition on diabetic veterans, the association of statin use and mortality in elderly veterans with and without diabetes, the impact of a new delivery system for human regular U-500 insulin in veterans with T2D, and the predictive power of plasma prekallikrein in myocardial infarction among participants in the Veterans Affairs Diabetes Trial.
1. Milyani R, Aparicio-Ugarriza R, Guerra JF, Salguero D, Mohammed YN, Valencia W, Florez H, Ruiz JG. 1451-P: The association of metformin with mortality in frail older veterans with diabetes. Diabetes 2019 June; 68(Supplement 1).
2. Thorson G, Patterson JM, Jorgensen K, Veigulis ZP. 904-P: Identification, diagnosis and treatment of prediabetes in veterans at VA Central Iowa. Diabetes 2019 June; 68(Supplement 1).
3. Raghavan S, Ho Y-L, Posner D, Vassy JL, Gagnon DR, Phillips LS, Wilson PW. 1460-P: Predicting atherosclerotic cardiovascular disease (ASCVD) risk in veterans with diabetes. Diabetes 2019 June; 68(Supplement 1).
4. Gosmanov AR, Gosmanova E. 1117-P: Metformin increases blood lactic acid in diabetic veterans with stage 3 CKD. Diabetes 2019 June; 68 (Supplement 1).