EAST ORANGE, NJ—As the VA increases its focus on minimizing hypoglycemia in veterans with type 2 diabetes, it expects that more physicians and veterans will consider using continuous glucose monitors to meet that goal.
As with other aspects of diabetes treatment at the VA, determining who would benefit from a continuous glucose monitor and which type would be best should start with a conversation between the physician and veteran, explained Leonard Pogach, MD, MBA, the VA’s national program director for Endocrinology and Diabetes. There are some general characteristics that indicate a veteran might benefit, however.
“Patients who are good candidates are those that are clinically insulinopenic (in the judgment of the prescribing clinician) and are on a multiple dose insulin regimens that necessitate frequent self-monitoring of blood glucose,” Pogach told U.S. Medicine.
That analysis aligns with the current International Consensus on Use of Continuous Glucose Monitoring which recommended that “CGM should be considered in conjunction with HbA1c for glycemic status assessment and therapy adjustment in all patients with type 1 diabetes and patients with type 2 diabetes treated with intensive insulin therapy who are not achieving glucose targets, especially if the patient is experiencing problematic hypoglycemia.”
Both Pogach and the consensus statement touch on one of its national priorities in treating veterans with diabetes—reducing the number and severity of hypoglycemic events. “CGM is most beneficial in addressing hypoglycemia—from recurrent milder hypoglycemic events that impact quality of life to serious hypoglycemia requiring third party assistance or medical treatment,” Pogach explained.
Depending on the device, a CGM could alert patients that their blood glucose is dropping or has entered hypoglycemic territory or it could let patients know that information when they check their sensors. A study that included both type 1 and type 2 diabetes patients on either multiple daily insulin injections or continuous subcutaneous insulin infusion found that patients who used continuous glucose monitoring spent about 60% less time in hypoglycemia than those who relied only on self-monitoring of blood glucose.1
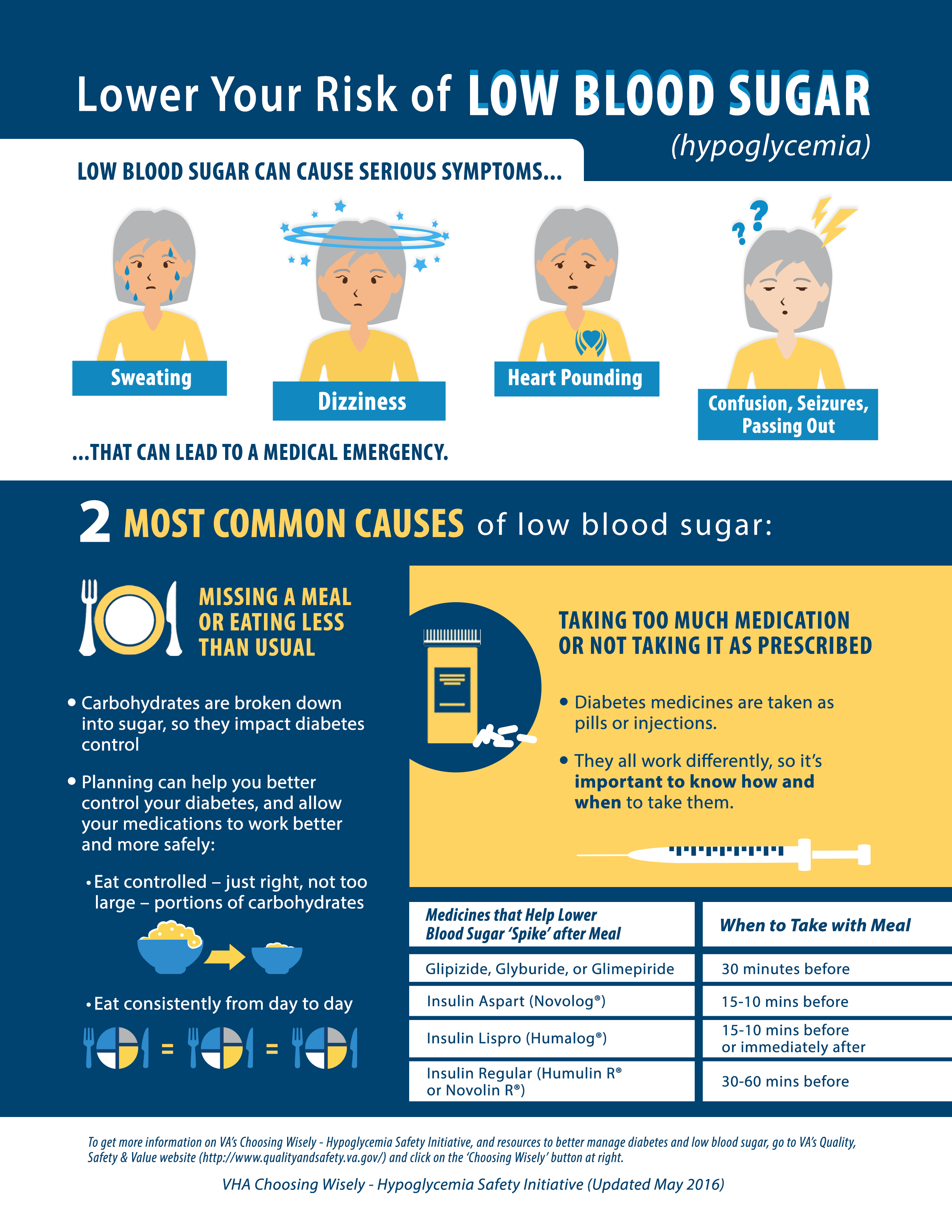
The VA is a national leader in preventing hypoglycemia among patients with diabetes, having launched the national Hypoglycemic Safety Initiative in 2014. The plan aims to increase awareness among clinicians and patients of the primary risk factors for hypoglycemia, including social determinants of health, health literacy and numeracy, comorbid conditions, timing of meals, cognitive impairment and overtreatment.
Detecting Hypoglycemia
According to the VA, about 50% of veterans who take medications to control their diabetes have comorbidities that increase their risk of serious hypoglycemia. Half of those veterans have documented A1c levels of less than 7%, which indicates “intensive management of hypoglycemia without significant benefit.” Hypoglycemia increases the risk of falls, accidents, confusion, unconsciousness, seizures and brain damage.
On the flip side, continuous glucose monitoring can also help patients who have blood sugar levels that are consistently too high, according to Pogach. “It can also benefit patients in achieving agreed upon glycemic goals despite adherence to their regimen; or for other individual reasons.”
A study in the Annals of Internal Medicine found that patients with type 2 diabetes who took multiple daily insulin injections and used a continuous glucose monitor for six months achieved greater reductions in A1c levels than patients who self-monitored. The DIAMOND trial enrolled 158 adults, with baseline A1c of 7.5% to 9.9%, who were randomly assigned to the two monitoring arms. Patients in the CGM arm saw their A1c levels decline from an average of 8.5% to 7.7%, while in those who performed standard blood glucose monitoring A1c dropped from a mean of 8.5% to 8.0%. Patients who had a baseline A1c greater than 9% experienced greater reduction, 1.4% compared to 0.7%.
An accompanying editorial noted that the modest improvement in A1c seen in the DIAMOND study could be attributed to minimal follow up and training on the devices, as anecdotal evidence and another trial found that when CGMs are paired with intensive diabetes education, A1c levels decreased more than 1.1%.2
Notably, 93% of the patients assigned to the CGM arm continued to use the device for the entire six months. Patients who used earlier versions of the devices sometimes found them bulky or difficult to use, but the technology has continued to improve, leading to a smaller profile and easier interpretation. The newer devices also have greater accuracy and fewer false alarms, so patients do not suffer from “alarm fatigue” that can lead them to discount warnings.
While the VA has not yet seen a notable jump in CGM use, “we expect that there will be an increased use of all FDA approved devices,” according to Pogach.
That would reflect trends seen elsewhere. Nationally, the use of CGMs is rising, “especially in patients on multiple daily insulin injections and on Medicare, since CMS covers these systems for patients with diabetes on multiple daily injections eligible for CGM,” Grazia Aleppo, MD, told U.S. Medicine. Aleppo is an endocrinologist at Northwestern University Feinberg School of Medicine with a focus on insulin pump therapy and CGM for type 1 and type 2 diabetics.

Advances seen in newer CGM systems have contributed to increased interest, she said. “The approval of Freestyle Libre, as well as Dexcom G6 will likely increase the adoption of CGM in view of the fact that both Libre and Dexcom G6 do not require any calibration and virtually eliminate the need to check blood glucose by fingerstick with the advantage of continuous glucose information.”
Continuous glucose monitors use a small tube placed under the skin and measures the glucose concentrations in the body’s interstitial fluid. While one of the advantages of CGM is a reduction in the number of times a patient must measure blood sugar levels by pricking their fingers and using a glucometer, earlier systems required regular calibration against the results seen by self-monitoring. The FDA approved the two newest CGMs to be used without self-monitoring blood glucose confirmation.
For Aleppo, the rapid evolution of the devices and the quality of information they provide make them useful for even more patients than the groups already identified by the VA and others. “In theory, any patient with type 2 diabetes could be a good candidate for CGM as it gives users dynamic on-demand information about glucose levels and fluctuations from food intake, exercise, etc. At this time, patients with type 2 diabetes on multiple daily insulin injections should be on CGM, in view of the benefits observed in reduction of HbA1c, increase of time spent in target range of 70-180 mg/dL and reduction of hypoglycemia.”
1. New JP, Ajjan R, Pfeiffer AF, Freckmann G. Continuous glucose monitoring in people with diabetes: the randomized controlled Glucose Level Awareness in Diabetes Study (GLADIS). Diabet Med. 2015 May;32(5):609-17.
2. Beck RW, Riddlesworth TD, Ruedy K, Ahmann A, Haller S, Kruger D, McGill JB, Polonsky W, Price D, Aronoff S, Aronson R, Toschi E, Kollman C, Bergenstal R; DIAMOND Study Group. Continuous Glucose Monitoring Versus Usual Care in Patients With Type 2 Diabetes Receiving Multiple Daily Insulin Injections: A Randomized Trial. Ann Intern Med. 2017 Sep 19;167(6):365-374.

