WASHINGTON—While the VA has declared preventing veteran suicide to be their top priority, veterans continue to attempt or commit suicide at VA healthcare facilities. Recent reports from the VA Inspector General’s Office suggest that the deficiencies that allow these incidents to occur are not always about providing appropriate mental healthcare but about failures in communication and organizational gaps between care teams.
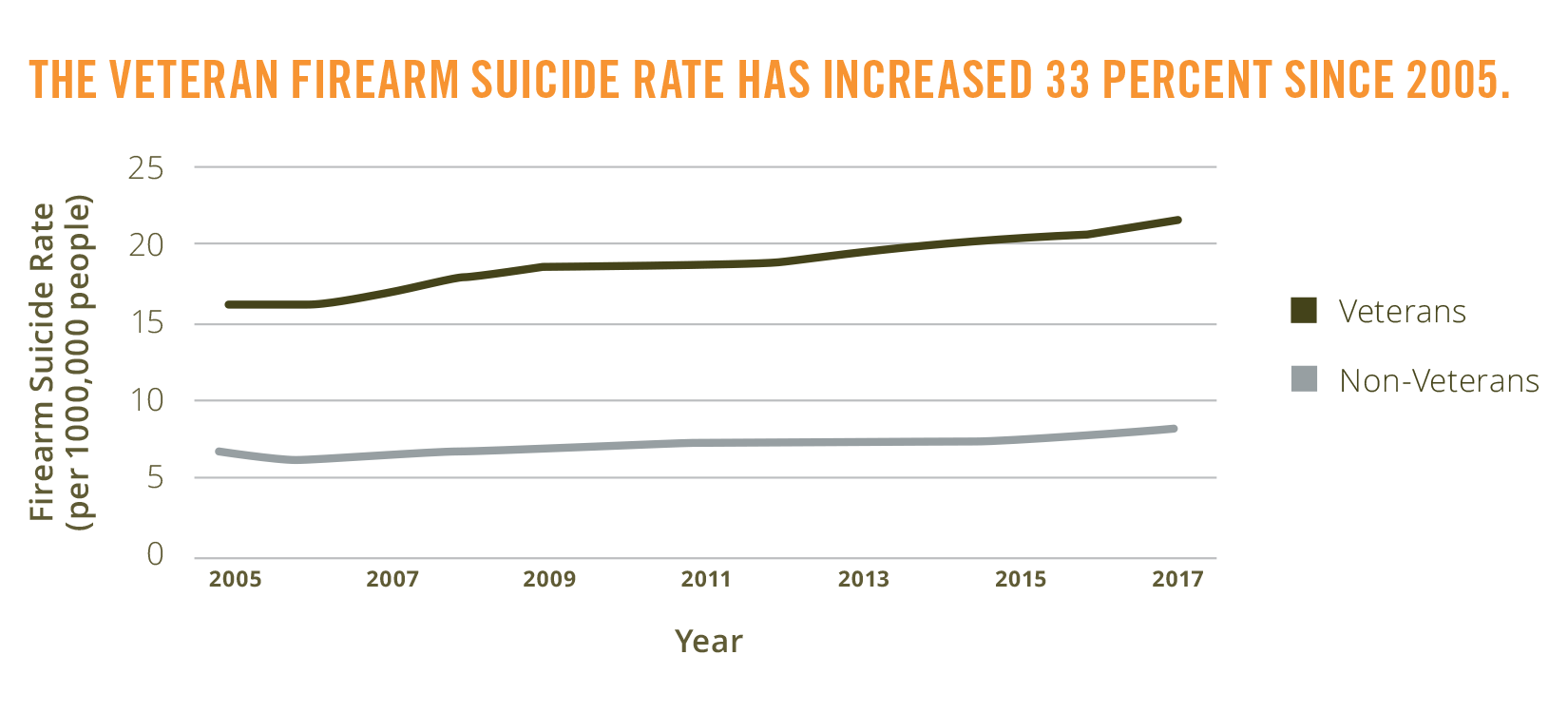
Veteran and non-veteran firearm suicide rates exclude suicides among people age 17 years old and under.
“Since the beginning of 2018, the VA Inspector General has published at least a dozen reports on facility security, environment of care, and a lack of care coordination at VA facilities,” declared Rep. Mark Takano (D-CA) at a House VA Committee hearing last month. “The IG found inadequate coordination of care to be an underlying theme in every one of its recently conducted reviews, whether it was a mental health treatment team, non-mental health providers during the discharge process, or by care providers for patients or their families.
“In one tragic instance at the Minneapolis VA Medical Center,” added Takano, the committee’s chairman, “staff failed to report on a patient’s suicidal ideation to the facility’s suicide prevention coordinator. In a different case at this same facility, the OIG determined that the VA’s inpatient treatment team failed to coordinate with the outpatient treatment team.”
Both of those incidents resulted in suicide.
“Tragic events are the most publicized and are typically understood to be the result of untreated, undertreated or unrecognized mental health disorders. Because of this, much of our work focuses on the complete healthcare journey of those veterans,” explained Julie Kroviak, MD, Deputy Assistant IG for Healthcare Inspections. “Our report identifies deficiencies in how VHA staff coordinated care for veterans, as well as the quality of the environment where veterans received that care.”
Communication Breakdown
The OIG team documented breakdowns in communication within the mental health treatment team, as well as between that team and other providers, and between VHA and the patient’s family and caregivers. Poor management of discharge and outpatient planning can put patients at risk of serious complications with devastating outcomes, Kroviak noted.
“While policies promoting effective communication may have been in place, staffing shortages, inconsistent training, and leadership failures compromised patient management,” she told legislators.
Questioned about severe shortages in mental health providers, Renee Oshinski, Deputy Under Secretary for Operations and Management, said, “We’ve made some tremendous progress in the last few years, however there are pockets where we still have difficulty trying to bring the staff on to the level that we need to support the demand…It’s a high growing area. We have a lot of veterans seeking care.”
Even when leadership roles are filled, that does not guarantee that on how to better prevent patient suicide will be addressed, however. The OIG has repeatedly reported on problems with the culture of specific VA facilities where complaints are ignored and, as a result, problems reoccur.
“Much of our recommendations are focused on filling leadership vacancies and other staff vacancies, but we’ve also identified in several high profile reports where staff members will complain and speak up and say this has not been consistently practiced. But the culture was such that after five or six times they stopped, because there was no action in place to really support effective leadership responding,” Kroviak explained.
She also impressed on the committee that, while OIG reports are usually responding to a specific incident, the biggest opportunity to prevent veteran suicide is before the veteran even considers the act.
“VHA’s efforts, including the Veterans Crisis Line, have largely been directed at crisis intervention,” she explained. “But the opportunity to intervene once a person decides on self harm is very short. Often less than an hour before the actual attempt. For veterans, it’s even more fraught with peril, because they are very likely to use firearms.”
According to suicide studies, the interim between the decision to complete suicide and the attempt is as short as one hour in over 70% of attempts. And while nearly half of all civilian suicide deaths involve a firearm, that number climbs to nearly 70% for veterans.
Mental health care must be paired with additional approaches to prevention, Kroviak said. One example of this effort on VA’s part is the department’s promotion of firearm safety, which urges veterans to secure guns with locks, remove firing pins, and store firearms where they cannot be easily accessed. This provides a suicidal veteran with more time to rethink their decision and increase the chances of an intervention.

