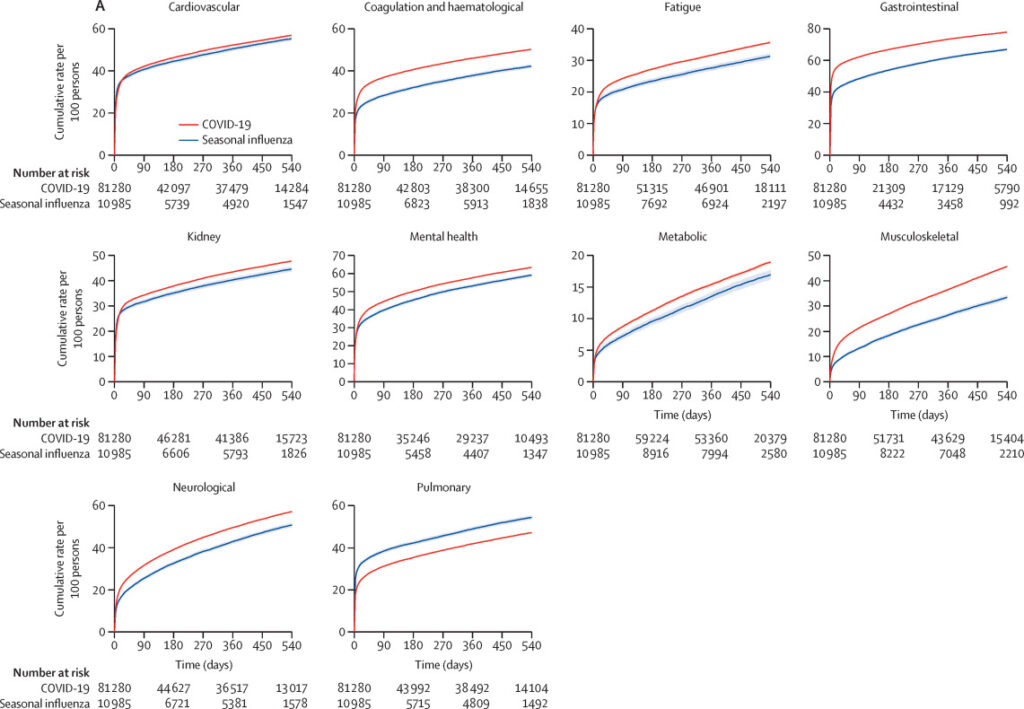
Click to Enlarge: Event rates of adverse health outcomes by organ system and across all organ systems in COVID-19 and seasonal influenza
(A) Event rates per 100 persons presented for the COVID-19 (red) and seasonal influenza (blue) groups in each organ system. (B) Disability-adjusted life-years (DALYs) per 100 persons presented for the COVID-19 (red) and seasonal influenza (blue) groups in each organ system. Shaded areas are 95% CIs. Source: The Lancet
ST. LOUIS — Clinicians are well aware of long COVID, the enduring health conditions caused by the SARS-CoV-2 virus’ ability to attack multiple organ systems. Now, VA researchers and others have determined that patients hospitalized with seasonal influenza also can suffer long-term, negative health effects, especially involving their lungs and airways.
The COVID-19 and flu viruses were similar in that, 18 months after infection, patients hospitalized for either of them faced an increased risk of death, hospital readmission and health problems in many organ systems, according to the study team from the VA Saint Louis Health Care System and Washington University School of Medicine in St. Louis. The time of highest risk was 30 days or later after initial infection, according to the report in The Lancet Infectious Diseases.1
“The study illustrates the high toll of death and loss of health following hospitalization with either COVID-19 or seasonal influenza,” said senior author Ziyad Al-Aly, MD, a clinical epidemiologist at the Saint Louis VAMC and Washington University. “It’s critical to note that the health risks were higher after the first 30 days of infection. Many people think they’re over COVID-19 or the flu after being discharged from the hospital. That may be true for some people. But our research shows that both viruses can cause long-haul illness.”
For the results published in The Lancet Infectious Diseases, statistical analysis lasted up to 18 months post-infection and included a comparative evaluation of risks of death, hospital admissions and 94 adverse health outcomes involving the body’s major organ systems.
“A review of past studies on COVID-19 versus the flu focused on a short-term and narrow set of health outcomes,” Al-Aly said. “Our novel approach compared the long-term health effects of a vast array of conditions. Five years ago, it wouldn’t have occurred to me to examine the possibility of a ‘long flu.’ A major lesson we learned from SARS-CoV-2 is that an infection that initially was thought to only cause brief illness also can lead to chronic disease. This revelation motivated us to look at long-term outcomes of COVID-19 versus flu.”
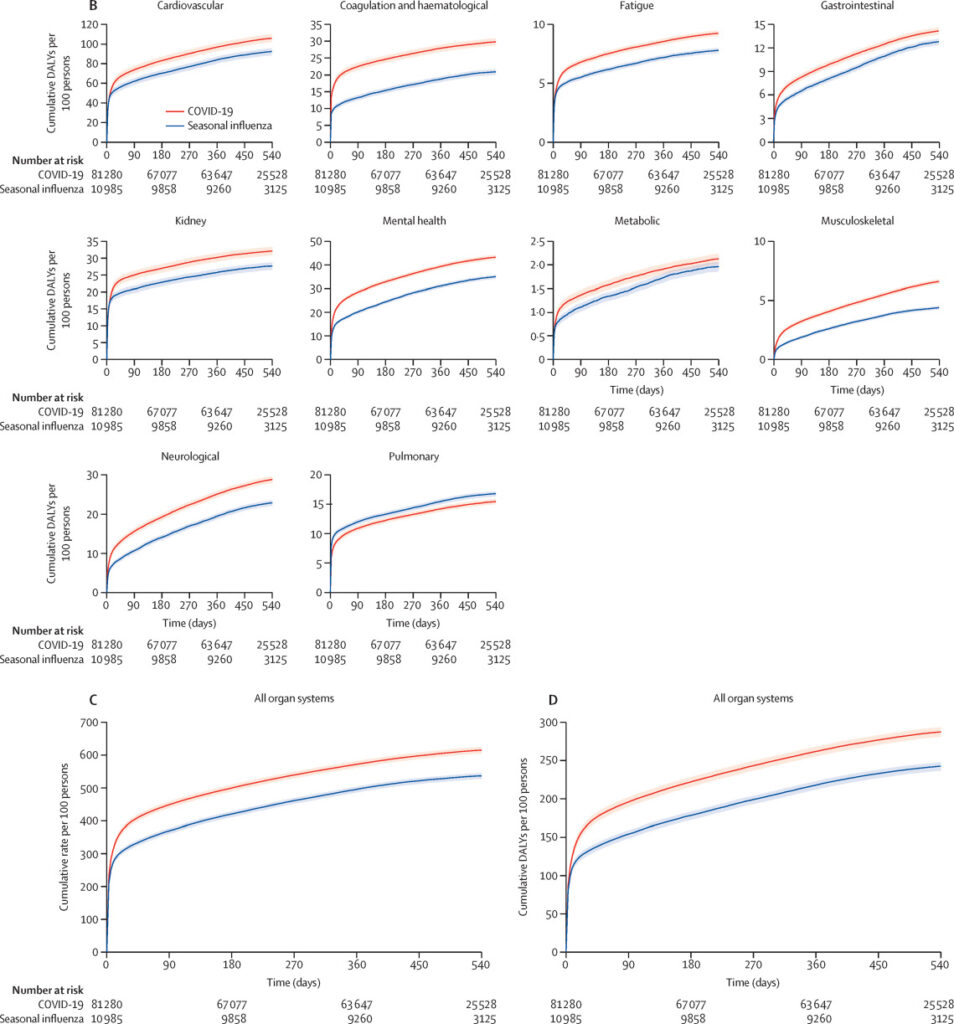
Click to Enlarge: Event rates of adverse health outcomes by organ system and across all organ systems in COVID-19 and seasonal influenza
(A) Event rates per 100 persons presented for the COVID-19 (red) and seasonal influenza (blue) groups in each organ system. (B) Disability-adjusted life-years (DALYs) per 100 persons presented for the COVID-19 (red) and seasonal influenza (blue) groups in each organ system. (C) Event rates per 100 persons presented for COVID-19 (red) and seasonal influenza (blue). (D) DALYs per 100 persons presented for COVID-19 (red) and seasonal influenza (blue). Shaded areas are 95% CIs. Source: The Lancet
Al-Aly said the study team sought to find out whether and to what degree those recovered from an initial flu infection also experience long-term health effects. “The big answer is that both COVID-19 and the flu led to long-term health problems, and the big aha moment was the realization that the magnitude of long-term health loss eclipsed the problems that these patients endured in the early phase of the infection,” he explained. “Long COVID is much more of a health problem than COVID, and long flu is much more of a health problem than the flu.”
He emphasized, however, that the overall risk and occurrence of death, hospital admissions and loss of health in many organ systems are substantially higher among COVID-19 patients than among those who have had seasonal influenza. “The one notable exception is that the flu poses higher risks to the pulmonary system than COVID-19,” Al-Aly said. “This tells us the flu is truly more of a respiratory virus, like we’ve all thought for the past 100 years. By comparison, COVID-19 is more aggressive and indiscriminate in that it can attack the pulmonary system, but it can also strike any organ system and is more likely to cause fatal or severe conditions involving the heart, brain, kidneys and other organs.”
For the cohort study, the VA’s databases were used to analyze data from 81,280 participants admitted to a hospital for COVID-19 between March 1, 2020, and June 30, 2022, and 10 985 participants admitted to a hospital for seasonal influenza between Oct 1, 2015, and Feb 28, 2019.
Results indicated that, over 18 months of follow-up, compared to seasonal influenza, the COVID-19 group had an increased risk of death (hazard ratio [HR] 1·51 [95% CI 1·45-1·58]), corresponding to an excess death rate of 8·62 (95% CI 7·55-9·44) per 100 persons in the COVID-19 group versus the influenza group.
Pulmonary Outcomes
In addition, comparative analyses of 94 prespecified health outcomes showed that COVID-19 had an increased risk of 68·1% (64 of 94) pre-specified health outcomes, while seasonal influenza was associated with an increased risk of 6·4% (six of 94) pre-specified health outcomes, including three out of four pre-specified pulmonary outcomes.
“Analyses of organ systems showed that COVID-19 had a higher risk across all organ systems except for the pulmonary system, the risk of which was higher in seasonal influenza,” the authors pointed out. The cumulative rates of adverse health outcomes across all organ systems were 615·18 (95% CI 605·17-624·88) per 100 persons in COVID-19 and 536·90 (527·38-544·90) per 100 persons in seasonal influenza, corresponding to an excess rate of 78·72 (95% CI 66·15-91·24) per 100 persons in COVID-19.
The total number of DALYs across all organ systems were 287·43 (95% CI 281·10-293·59) per 100 persons in the COVID-19 group and 242·66 (236·75, 247·67) per 100 persons in the seasonal influenza group, corresponding to 45·03 (95% CI 37·15-52·90) higher DALYs per 100 persons in COVID-19.
Compared to seasonal influenza, COVID-19 also had an increased risk of hospital readmission (excess rate 20·50 [95% CI 16·10-24·86] per 100 persons) and admission to intensive care (excess rate 9·23 [6·68-11·82] per 100 persons).
“Although rates of death and adverse health outcomes following hospital admission for either seasonal influenza or COVID-19 are high, this comparative analysis shows that hospital admission for COVID-19 was associated with higher long-term risks of death and adverse health outcomes in nearly every organ system (except for the pulmonary system) and significant cumulative excess DALYs than hospital admission for seasonal influenza,” the study concluded. “The substantial cumulative burden of health loss in both groups calls for greater prevention of hospital admission for these two viruses and for greater attention to the care needs of people with long-term health effects due to either seasonal influenza or SARS-CoV-2 infection.”
“Our findings highlight the continued need to reduce the risk of hospitalization for these two viruses as a way to alleviate the overall burden of health loss in populations,” Al-Aly said. “For both COVID-19 and seasonal influenza, vaccinations can help prevent severe disease and reduce the risk of hospitalizations and death. Optimizing vaccination uptake must remain a priority for governments and health systems everywhere. This is especially important for vulnerable populations, such as the elderly and people who are immunocompromised.”
In both COVID-19 and the flu, more than half of death and disability occurred in the months after infection, not the acute phase, defined as the first 30 days.
“The idea that COVID-19 or flu are just acute illnesses overlooks their larger long-term effects on human health,” Al-Aly emphasized. “Before the pandemic, we tended to belittle most viral infections by regarding them as somewhat inconsequential: ‘You’ll get sick and get over it in a few days.’ But we’re discovering that is not everyone’s experience. Some people are ending up with serious long-term health issues. We need to wake up to this reality and stop trivializing viral infections and understand that they are major drivers of chronic diseases.”
- Xie Y, Choi T, Al-Aly Z. Long-term outcomes following hospital admission for COVID-19 versus seasonal influenza: a cohort study. Lancet Infect Dis. 2023 Dec 14:S1473-3099(23)00684-9. doi: 10.1016/S1473-3099(23)00684-9. Epub ahead of print. PMID: 38104583.

