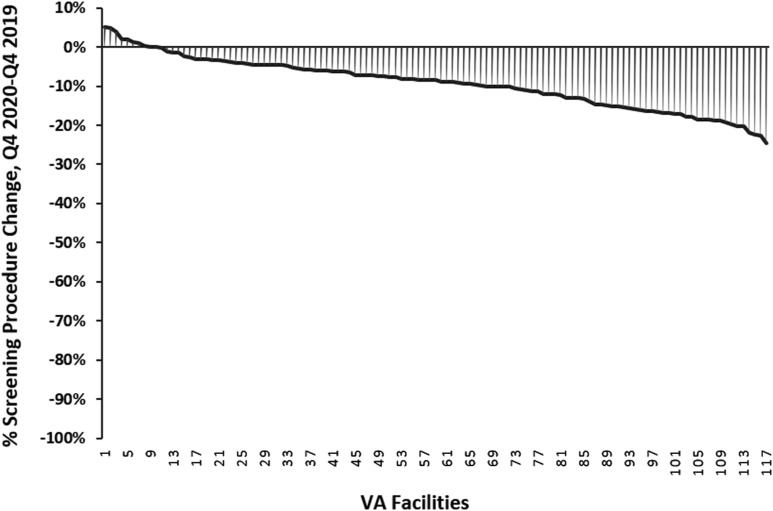
Click to Enlarge: Adjusted change in facility-level proportion of screening colonoscopies pre-COVID (fourth quarter [Q4] 2019) vs COVID (Q4 2020) by facility (highest to lowest).
ANN ARBOR, MI ― Backlogs in high-volume gastrointestinal endoscopic procedures, such as colonoscopy, occurred during the current COVID-19 pandemic, especially in the early days.
A new study in the journal Gastroenterology pointed out that the inability to perform that screening is projected to lead to a rise in avoidable colorectal cancers. “Almost one-third of colonoscopies performed in Veterans Health Administration (VHA), the largest integrated health system in the United States, are for screening,” according to the authors from the VA Ann Arbor, MI, Healthcare System and the University of Michigan Health System.1
The article pointed out, however, that colonoscopy is not the only option for colorectal cancer (CRC) screening. It explained that the U.S. Preventive Services Task Force recommends several different testing modalities, including annual fecal immunochemical testing (FIT), as alternatives to colonoscopy for average-risk screening.
“Future work should focus on developing multilevel implementation strategies to provide facilities with effective tools to enhance uptake and sustainability of stool-based CRC screening to reduce colonoscopy demand and improve overall endoscopy access for high-need patients, particularly in integrated healthcare systems and other settings with limited endoscopy access,” the authors emphasized.
Their recommendations were based on a recent simulation study that projected how increased FIT-based screening during COVID-19 could mitigate the consequences of reduced screening rates on CRC outcomes during the pandemic.
“Such an approach also could address longer-term endoscopy access challenges in settings where endoscopy demand exceeds capacity,” according to the report. “This is particularly important considering recent changes to US Preventive Services Task Force guidelines recommending initiating screening at age 45 (previously age 50). In the VHA alone, this change is estimated to increase the number of screening-eligible patients by 280,000, further exacerbating existing and creating new endoscopy access challenges.”
In March 2020, the VHA issued a national directive mandating preferential use of stool-based CRC screening in average-risk patients during the pandemic, at least partly to reduce endoscopy demand during the pandemic.
To better understand the situation, the authors conducted a retrospective cohort study of veterans undergoing screening colonoscopy from October to December 2019 (“pre-COVID”) and October to December 2020 (“COVID”).
The researchers calculated the overall and facility-level proportions of all colonoscopies performed for screening during each period, and the change in facility-level proportion pre-COVID and COVID. Results indicated that, during the study period, 99,595 total colonoscopies were performed at 117 VHA facilities. Of these, 28,082 (28.2%) were screening colonoscopies (pre-COVID, 18,681; COVID, 9401).
The study found that, system-wide, a 9.3% decrease (95% confidence interval [CI], –10.5% to –8.1%) in the mean (adjusted) facility-level proportion of screening procedures pre-COVID and COVID occurred. “Most facilities modestly decreased screening colonoscopy use in the COVID period, with wide variation across facilities (interquartile range, –14.8% to –4.6%),” the authors wrote. “At the same time, average monthly FIT volume increased by 7.9% before and after COVID-19 (pre-COVID, 31,604 FIT per month; COVID, 34,109 FIT per month).”
The study pointed out that most VHA facilities included in their analysis were high complexity and academically affiliated, explaining, “Higher complexity facilities achieved larger relative decreases in screening colonoscopy use than the lowest complexity facilities. However, even these higher complexity facilities decreased screening colonoscopy use by only ∼25%. Similarly, academically affiliated facilities achieved larger relative reductions in screening colonoscopy use (–28%; 95% CI, –33% to –22%) than non-academically affiliated facilities (–15%; 95% CI, –23% to –6%).”
The review also determined that facilities which had failed to regain their pre-COVID capacity by the fourth quarter of 2020 were no more likely to decrease screening colonoscopy use than those that had regained their capacity (P = .8231), with the proportion of screening procedures increaseing0.4% (95% CI, –3% to 4%) for every 10% additional regained capacity. That rate was not affected by geographic region, the researchers advised.
“Although we found a modest (9.3%) decrease in the overall proportion of screening procedures by the fourth quarter of 2020, VHA facilities clearly did not maximize the opportunity to accomplish a marked, system-wide reduction in screening colonoscopy demand by shifting to an underused, evidence-based alternative screening modality (FIT),” the authors concluded. “This occurred despite a national VHA policy directive strongly encouraging widespread adoption of a stool-based CRC screening strategy to enhance overall endoscopy access.”
The study also uncovered significant facility-level variation, with the greatest reduction in screening colonoscopy use occurring at higher complexity, academically affiliated sites.
The researchers posited that the modest response occurred because some sites might have been unaware of the national directive strongly encouraging systematic adoption of a stool-based screening strategy, “perceived more pressing priorities and/or failed to appreciate the link between reducing screening colonoscopy volume and addressing their acute endoscopy access challenges.” In addition, the facilities might not have had collaborative relationships between gastroenterology and primary care and leadership might have lacked the time to remedy that, they said.
“Although extreme pandemic-related care disruptions provided short-term motivation for change at these sites, these data suggest that whatever changes facilities were able to make in response to acute COVID-19–related resource constraints and the national directive were not and will not be sustainable in the long term,” the authors concluded. “Sustainability of this facility-level stool-based screening strategy will require a more systematic approach that leverages principles of implementation science, requires culture change, and promotes greater stakeholder engagement. Accomplishing such culture change and stakeholder engagement will necessitate multimodal strategies including collaboration with frontline providers and patients at the facility level, measurement of performance, and feedback.”
- Adams MA, Kurlander JE, Gao Y, Yankey N, Saini SD. Impact of Coronavirus Disease 2019 on Screening Colonoscopy Utilization in a Large Integrated Health System. Gastroenterology. 2022 Jun;162(7):2098-2100.e2. doi: 10.1053/j.gastro.2022.02.034. Epub 2022 Feb 24. PMID: 35219698; PMCID: PMC8867975.

