Study Questions Accuracy of Pulse Oximeter Measurements
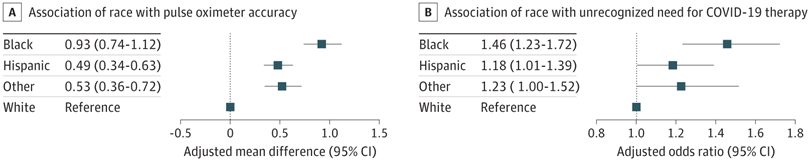
Click to Enlarge: Other racial and ethnic minority patients included Asian, Native American or Alaskan Native, Hawaiian or Pacific Islander, and patients with another race or ethnicity. A. Pulse oximeter accuracy defined as mean difference between pulse oximeter saturation (SpO2) and arterial oxygen saturation (SaO2). B. Delayed recognition defined as first SaO2 measurement below 94% despite SpO2 of 94% or above. Source: JAMA Network Open
BALTIMORE, MD — The overestimation of oxygen saturation by pulse oximetry in patients led to the delay of COVID-19 treatment and potentially increased hospital readmissions, according to a new study.
The report in JAMA Network Open suggests that Black patients were more likely to have an unrecognized need for therapy, and that led to possible population-level health disparities.1
The new cohort study, led by Johns Hopkins University School of Medicine researchers, involved 24,504 patients with concurrently measured pulse oximetry and arterial oxygen saturation. It found that pulse oximeters more commonly overestimated arterial oxygen saturation in patients from minority racial and ethnic groups and led to delayed recognition of the need for COVID-19 therapy among Black patients compared with white patients.
Taking part in the study was the Center for Innovations in Quality, Effectiveness, and Safety at the Michael E. DeBakey VAMC in Houston.
Focusing on a subset of 8,635 patients without immediate need for therapy on admission, “overestimation of oxygen saturation by pulse oximetry was associated with delayed delivery of COVID-19 therapy and increased risk of hospital readmission, irrespective of patient race,” the study pointed out.
The study team advised that its results confirm the possibility of racial and ethnic disparities in the measurement of oxygen saturation by pulse oximetry, the risk of hospital admission is increased, regardless of patient race.
“Many pulse oximeters have been shown to overestimate oxygen saturation in persons of color, and this phenomenon has potential clinical implications,” the study team noted, adding that the relationship between overestimation of oxygen saturation with the timing of COVID-19 medication delivery and clinical outcomes had been unclear.
That’s why the investigators sought to investigate the association between overestimation of oxygen saturation by pulse oximetry and delay in administration of COVID-19 therapy, hospital length of stay, risk of hospital readmission and in-hospital mortality.
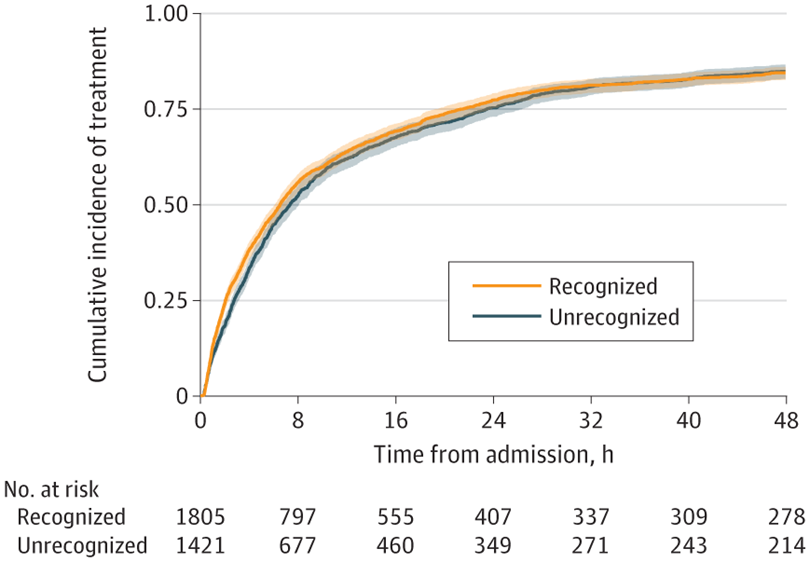
Click to Enlarge: Comparison of patients with COVID-19 admitted after July 1, 2020, with first arterial oxygen saturation (SaO2) measurement below 94% who had recognized or unrecognized need for COVID-19 therapy (concurrent pulse oximeter saturation [SpO2] at 94% or 94% and higher, respectively). Source: JAMA Network Open
In addition, a subset of patients was admitted after July 1, 2020, without immediate need for COVID-19 therapy based on pulse oximeter saturation (SpO2 levels of 94% or higher without supplemental oxygen).
Race and Ethnicity
The focus was on self-reported race and ethnicity, the difference between concurrent SaO2 and pulse oximeter saturation (SpO2) within 10 minutes, and the initially unrecognized need for COVID-19 therapy (first SaO2 reading below 94% despite SpO2 levels of 94% or above).
Patients included in the age had a median age of 63.9 and were 41.9% female. The greatest percentage was white, 41.1%, followed by Hispanic, 32.2%, and Black, 16%, with 10.4% being Asian, Native American or Alaskan Native, Hawaiian or Pacific Islander or another race or ethnicity.
The study reported that “pulse oximetry overestimated SaO2 for Black (adjusted mean difference, 0.93 [95% CI, 0.74-1.12] percentage points), Hispanic (0.49 [95% CI, 0.34-0.63] percentage points), and other (0.53 [95% CI, 0.35-0.72] percentage points) patients compared with White patients. In a subset of 8,635 patients with a concurrent SpO2-SaO2 pair without immediate need for COVID-19 therapy.”
Black patients were much more likely to have pulse oximetry values that “masked” any indication to receive COVID-19 therapy compared with White patients (adjusted odds ratio [aOR], 1.65; 95% CI, 1.33-2.03), the researchers pointed out, adding, “Patients with an unrecognized need for COVID-19 therapy were 10% less likely to receive COVID-19 therapy (adjusted hazard ratio, 0.90; 95% CI, 0.83-0.97) and higher odds of readmission (aOR, 2.41; 95% CI, 1.39-4.18) regardless of race (P for interaction =0 .45 and P = 0.14, respectively). There was no association of unrecognized need for COVID-19 therapy with in-hospital mortality (aOR, 0.84; 95% CI, 0.71-1.01) or length of stay (mean difference, -1.4 days; 95% CI, -3.1 to 0.2 days).”
Background information in the article recounted how pulse oximetry, which noninvasively estimates arterial oxygen saturation, was first developed during the 1970s and has become ubiquitous in healthcare settings and influences clinical decision-making.
“During the COVID-19 pandemic, oxygen saturation thresholds were used to define disease severity, making the pulse oximeter particularly important for triage and treatment decisions,” the authors wrote.
Observational data and laboratory studies suggest, however, that pulse oximeters “systematically overestimate arterial oxygen saturation among patients from minority racial and ethnic groups, leading to a greater risk of occult hypoxemia, generally defined as a true arterial oxygen saturation (SaO2) below 88% with an oxygen saturation by pulse oximetry (SpO2) in a normal range above 92%. The presence of occult hypoxemia has been associated with lower rates of supplemental oxygen among critically ill patients.”
- Fawzy A, Wu TD, Wang K, et al. Clinical Outcomes Associated With Overestimation of Oxygen Saturation by Pulse Oximetry in Patients Hospitalized With COVID-19. JAMA Netw Open. 2023;6(8):e2330856. doi:10.1001/jamanetworkopen.2023.30856


