Study Suggests VHA Did a Better Job of Providing COVID-19 Care

In May 2020, soldiers and airmen of the Mississippi National Guard gather at the employee entrance to the G.V. (Sonny) Montgomery VAMC in Jackson, MS, to honor civilian healthcare workers during National Nurses Week. Guardsmen cheered for VA employees as they entered and exited the hospital during morning shift change and thanked them for their work during the COVID-19 pandemic. Now, a new study quantifies just how well those employees did. U.S. Army National Guard photo by Spc. Christopher M. Shannon II
BOSTON — Despite older age and more potentially dangerous comorbidities, veterans receiving VA care fared better last year than those treated in community healthcare systems during the COVID-19 pandemic, according to a new study.
The report in The Lancet Regional Health-Americas pointed out that more U.S. veterans died in 2020 than in earlier years but that the increase lagged the mortality rise for the general population.1
The study was conducted by researchers from Boston University School of Public Health, the VA Boston Healthcare System and Vanderbilt University Medical Center in Nashville, TN.
Researchers reported that deaths among U.S. veterans receiving VA care increased 16% in 2020, but the increase among the general population was 23%. That signaled that, despite veterans having a higher number of comorbidities, such as older age, hypertension, diabetes and obesity, the VA system apparently performed better at preventing COVID-19 deaths, the authors said.
“This suggests the Veterans Health Administration performed better than expected,” advised Kevin Griffith, PhD, assistant professor in the Department of Health Policy at VUMC who studies the VA. “Despite VHA-enrolled veterans having a higher prevalence of risk factors for severe COVID-19 illness, their rate of excess deaths was markedly lower than what was observed in the general population.”
The study noted that U.S. veterans are, in general, experiencing increases in both COVID-19 and non-COVID-19 mortality. “Veterans may be more susceptible to the pandemic than the general population due to their higher comorbidity burdens and older age, but no research has examined if trends in excess mortality differ between these groups,” the authors wrote.
They added that, because individual-level data on demographics, comorbidities, and deaths are provided in near-real-time for all enrollees of the VHA, they had a unique opportunity to identify excess mortality in 2020 and compare that to community statistics.
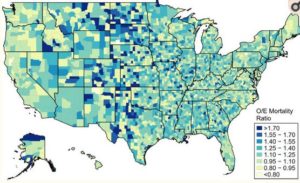
Click To Enlarge: County-level estimates of excess all-cause mortality during 2020, Source: Authors’ analysis of data from the Veterans Health Administration’s Corporate Data Warehouse. Notes: The figure displays observed-to-expected (O/E) mortality ratios for 2020, defined as total observed deaths versus total deaths predicted by the regression model. O/E ratios were estimated via a covariate-adjusted quasi-likelihood Poisson regression with county fixed effects and 5-fold cross validation as described in the text.
The study team collected VHA administrative data on demographics and comorbidities for 11.4 million enrollees during 2016-2020. For comparison, it then estimated county-level excess veteran mortality during 2020 and correlated these estimates with local rates of COVID-19 confirmed cases and deaths.
“We developed sub-national estimates of excess mortality associated with the pandemic and shared our data as a resource for researchers and data journalists,” the researchers explained. “Despite veterans’ greater likelihood of risk factors associated with severe COVID-19 illness, their excess mortality rate was slightly lower than the general population. Consistent access to health care and the rapid expansion of VHA telemedicine during the pandemic may explain this divergence.”
Researchers suggested their study could help other investigators examine excess mortality attributable to the pandemic and, “using our approach, help evaluate whether interventions may have successfully moderated the effects of the pandemic. Moreover, this work provides a framework to model excess mortality in future waves of the COVID-19 pandemic or pandemics of other novel infectious viruses.”
Avoidance of Care
Background information in the article noted that, In the United States, an estimated 40% of adults avoided care during the COVID-19 pandemic, including 12% who avoided emergency care and 31% who avoided routine care. “Early evidence suggests that, while some of the forgone care was low value, some was high value,” the authors pointed out. “Timely access to care is an important determinant of both short- and long-term health, and disruptions in healthcare access may increase the risk of avoidable morbidity and mortality for other conditions. Additionally, in some regions, hospitals’ inpatient and critical care facilities faced overcrowding during the pandemic’s peak, which may have led to increased mortality and worsened health outcomes.”
“We know that, when hospitals and ICUs are full, both sicker and healthier patients die at higher rates for many diseases, not just COVID,” Griffith said.
The researchers added that prior studies estimate that, nationally, all-cause mortality among the general population increased by approximately 23% from March 2020 through the end of the year. “However, there is a dearth of research using individual-level data or on subnational excess mortality estimates,” they said.
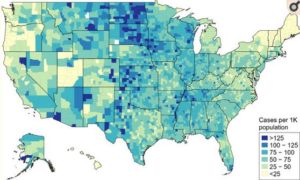
Click To Enlarge: County-level burden of confirmed COVID-19 cases in the general population during 2020, Source: Authors’ analysis of data from the Johns Hopkins Coronavirus Resource Center. Notes: The figure displays data on COVID-19 cases for the general population and is not veteran-specific.
The study applauded VHA for implementing “an early, nationwide response to limit the spread of the pandemic. While VHA inpatient utilization fell by 42% during the pandemic’s early months, telehealth encounters grew by 556% from March to April 2020. VHA electronic health records also become available to researchers in near real-time. As such, the VHA is an ideal system within which to examine the impact of the pandemic on excess all-cause mortality.”
How well veterans with COVID-19 varied geographically, however. The study pointed out that veterans living in states across the Great Plains faced heightened mortality risks in 2020, where cases of COVID-19 were also higher per 1,000 population. Overall, the study estimates that 426,069 veterans died in 2020, which was 51,436 more than what the models had predicted if a global pandemic hasn’t occurred.
Lead author Yevgeniy Feyman, a doctoral candidate at BU, advised that, while no absolute explanation exists for why VA had a smaller increase in deaths compared to the general population, a possible reason is that the VA deployed useful tools early on as the pandemic impacted the nation’s healthcare system.
“For instance, many in the U.S. lost or were forced to switch health insurance plans due to layoffs—while in the VA access isn’t conditional on employment,” Feyman said. “The VA mounted a large, national response to COVID-19 early on, even in areas where the pandemic wasn’t bad yet and had existing telehealth infrastructure they could rapidly scale that many community-based providers did not already have in place.”
The VA helped fund the study, and the authors concluded that their results will be helpful to the agency, “Our work provides valuable insights into the experience and needs of veterans and may be used to help VHA leadership and other integrated health systems forecast changes in healthcare access and utilization demand for patients at continued high risk.”
-
Feyman Y, Auty SG, Tenso K, Strombotne KL, Legler A, Griffith KN. County-Level Impact of the COVID-19 Pandemic on Excess Mortality Among U.S. Veterans: A Population-Based Study. Lancet Reg Health Am. 2021 Oct 30:100093. doi: 10.1016/j.lana.2021.100093. Epub ahead of print. PMID: 34778864; PMCID: PMC8577544.

