Click to Enlarge: Association of CLD with 30-Day Severity of Illness Outcomes in COVID-19+ Veterans
Source: Annals of the American Thoracic Society
SEATTLE — Veterans with chronic lung diseases, particularly idiopathic pulmonary fibrosis (IPF), other interstitial lung diseases (ILD) and chronic obstructive pulmonary disease (COPD), have an increased risk of experiencing more severe 30-day outcomes with COVID-19, according to a recent study.
The study published in the Annals of the American Thoracic Society determined the risk, both overall and by type of chronic lung disease, for severity of COVID-19 outcomes. The authors, affiliated with VA Puget Sound Healthcare System in Seattle, wrote that they pursued this study because “chronic lung diseases have been associated with a risk for more severe manifestations and death with COVID-19.”1
“The virus that causes COVID-19 targets the respiratory tract, so people with chronic lung diseases might be particularly vulnerable to severe illness and poor outcomes,” : lead author Kristina Crothers, MD, told U.S. Medicine. “We wanted to see if this was true for veterans who have a high prevalence of chronic lung disease. The large, comprehensive VA dataset allowed us to compare outcomes of different chronic lung diseases to understand which had the biggest impact, including less common ones like various interstitial lung diseases.”
The researchers used data from the VHA’s Corporate Data Warehouse and the VA COVID-19 Shared Data Resource to determine the risk associated with chronic lung diseases, including COPD (mild or severe), asthma (mild, active or severe), IPF, sarcoidosis and other ILDs, for outcomes among veterans with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-positive tests between March 1, 2020 and April 30, 2021. The study included 208,283 veterans with COVID-19, and 35,587 (17%) had chronic lung diseases.
To determine the study’s results, the authors “used multinomial regression to estimate risk of four mutually exclusive COVID-19 outcomes within 30 days: outpatient management, hospitalization, hospitalization with indicators of critical illness, or death. They calculated risk for each outcome between those with and without chronic lung diseases, and described clinical and laboratory abnormalities by chronic lung diseases in those hospitalized.”
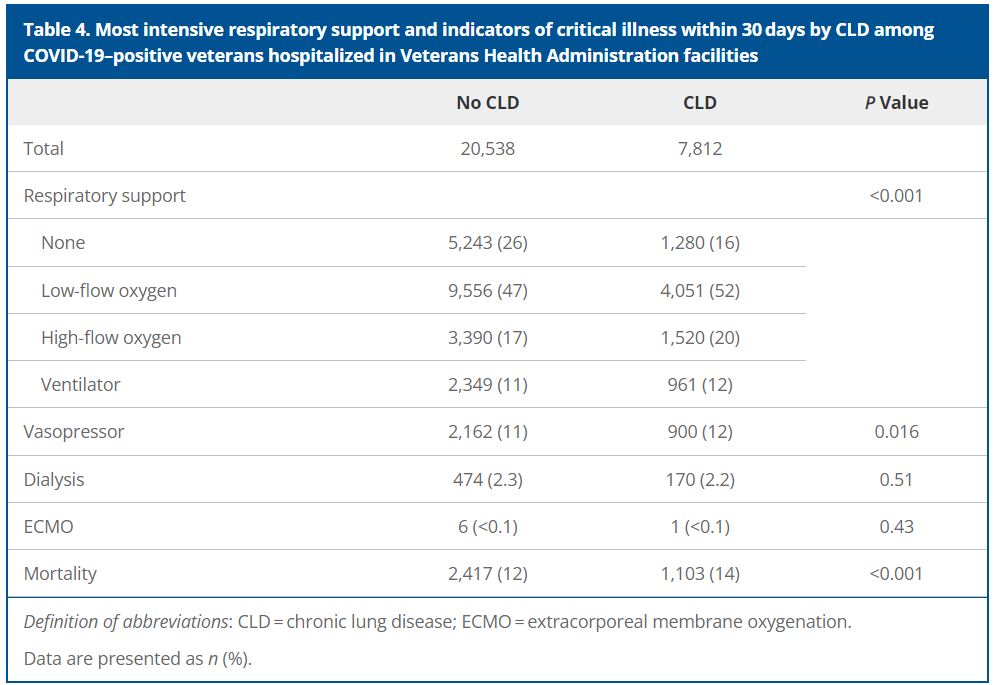
“We found that veterans with chronic lung diseases were more likely to have severe COVID-19,” explained Crothers, who is with the VA Puget Sound Healthcare System and the University of Washington, both in Seattle. “We considered four outcomes within 30 days: mild illness if they were outpatients; moderate if they were hospitalized without critical illness; critical if they were hospitalized with critical illness; and fatal if they died. Veterans with COVID-19 were less likely to be outpatients and more likely to be hospitalized, critically ill and to die. Hospitalized patients with chronic lung disease and COVID-19 had lower average temperature, white blood cell count and platelet count. They were also older and had more of other illnesses. Adjusting for these factors reduced, but did not eliminate, the differences in severity outcomes.”
When considering different types of chronic lung diseases, “veterans with IPF, ILDs and COPD were more likely to have severe 30-day outcomes. The association with more severe outcomes was stronger in individuals under age 65,” Crothers added.
IPF Patients Most at Risk
“Individuals with chronic lung diseases are at risk for more severe outcomes of COVID-19,” she pointed out. . “The strongest risk was with idiopathic pulmonary fibrosis, especially in those under age 65. Individuals with other interstitial lung diseases and COPD were also at risk of more severe outcomes but to a lesser extent. In general, the risk of a critical outcome was more significant than the risk of a fatal outcome among veterans with chronic lung diseases.”
The study reported that “veterans with chronic lung diseases were significantly less likely to have mild COVID-19 (-4.5%; adjusted risk ratio [aRR], 0.94; 95% confidence interval [CI], 0.94-0.95), and more likely to have a moderate (+2.5%; aRR, 1.21; 95% CI, 1.18-1.24), critical (+1.4%; aRR, 1.38; 95% CI, 1.32-1.45), or fatal (+0.7%; aRR, 1.15; 95% CI, 1.10-1.20) outcome.”
In addition, the researchers found that “IPF was most strongly associated with COVID-19 severity, especially mortality (+3.2%; aRR, 1.69; 95% CI, 1.46-1.96), followed by other ILDs and COPD, while asthma was less likely to be associated with severity of COVID-19. In veterans younger than 65 years old, worse COVID-19 outcomes were generally more likely with IPF, sarcoidosis and other ILDs.”
The study results indicated that, compared with no CLD, veterans with CLD were older and had more comorbidities.
“Hospitalized veterans with CLD were more likely to have low temperature, mean arterial pressure, oxygen saturation, and leukopenia and thrombocytopenia and were more likely to receive oxygen, mechanical ventilation, and vasopressors,” the authors advised. In addition, they noted that veterans with CLD were significantly less likely to have mild COVID-19 (-4.5%; adjusted risk ratio [aRR], 0.94; 95% confidence interval [CI], 0.94-0.95), and more likely to have a moderate (+2.5%; aRR, 1.21; 95% CI, 1.18-1.24), critical (+1.4%; aRR, 1.38; 95% CI, 1.32-1.45), or fatal (+0.7%; aRR, 1.15; 95% CI, 1.10-1.20) outcome.
IPF was most strongly associated with COVID-19 severity, especially mortality (+3.2%; aRR, 1.69; 95% CI, 1.46-1.96), followed by other ILDs and COPD, and asthma was less likely to be associated with severity of COVID-19. In veterans younger than age 65 years, worse COVID-19 outcomes were generally more likely with IPF, sarcoidosis and other ILDs.
The study’s results offer insight into “the risk of different chronic lung diseases with severity of COVID-19 outcomes and can help inform considerations of healthcare utilization and prognosis,” according to the authors.
For healthcare professionals who are treating veteran patients with chronic lung diseases, being aware of these findings can help them “consider therapies for patients with chronic lung disease and COVID-19, decide on hospitalization and need for intensive care, and assess prognosis,” Crothers suggested.
She said the researchers “don’t know if chronic lung diseases impact COVID-19 risk the same way as newer variants of SARS-CoV-2 or what the impact on developing long COVID might be. As a result, the VA encourages patients in high-risk groups to receive updated COVID-19 vaccinations.”
“In addition to vaccination, patients with chronic lung diseases may want to consider the risks and benefits of attending events that are higher risk for contracting COVID-19 when infection rates are high in their area, especially if they do not wear a mask,” Crothers advised.
- Crothers K, Adams SV, Turner AP, Batten L, Nikzad R, Kundzins JR, Fan VS. COVID-19 Severity and Mortality in Veterans with Chronic Lung Disease. Ann Am Thorac Soc. 2024 Jul;21(7):1034-1043. doi: 10.1513/AnnalsATS.202311-974OC. PMID: 38530061.


