Veteran Study Was ‘Eye-Opening’ for Researchers
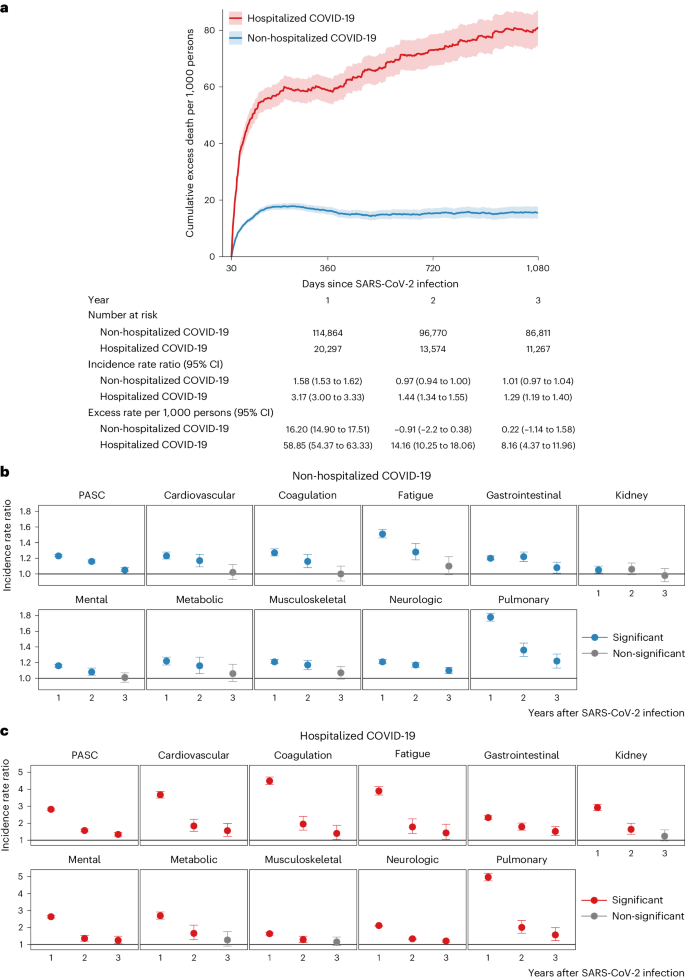
Click to Enlarge: Cumulative excess death rate and incidence rate ratio of PASC in COVID-19 groups by care setting of the acute phase. Source: Nature Medicine
ST. LOUIS — The long-term effects of COVID-19 might last longer and manifest themselves later than was previously thought, according to a new study that followed patients for three years after their initial illness.
The research from the VA St. Louis Healthcare System and Washington University School of Medicine in St. Louis provided important insights about the long-term effects of infection with SARS-CoV-2 and potentially other viruses as well, said lead author Ziyad Al-Aly, MD. It was published recently in Nature Medicine.1
Al-Aly and his colleagues, who had been tracking and reporting on the effects of SARS-CoV-2 from the pandemic’s beginning, wanted to know how COVID-19 patients fared in their third year after infection.
To do so, they used VA national healthcare databases to develop a cohort of 135,161 veterans who survived the first 30 days of COVID-19 (20,297 of whom had been hospitalized with COVID-19 and 101,054 who had not) and a control group of 5,206,835 users of the VA healthcare system with no evidence of SARS-CoV-2 infection. To ensure three-year follow-up, these cohorts were enrolled between March and December 2020, an era that predated the availability of COVID-19 vaccines and antivirals but when the ancestral SARS-CoV-2 virus predominated.
The cohorts were followed longitudinally for three years to estimate the risks of death and incident sequelae of SARS-CoV-2 throughout the three-year follow-up and cumulatively at three years in mutually exclusive groups according to care setting (nonhospitalized and hospitalized) of the acute phase of the disease.
The results showed that, among nonhospitalized individuals, the increased risk of death was no longer present after the first year of infection. Among hospitalized patients, however, the risk of death declined but remained significantly elevated in the third year after infection. The risk of sequelae declined but remained substantial in the third year. “Altogether, our findings show reduction of risks over time, but the burden of mortality and health loss remains in the third year among hospitalized individuals,” the researchers wrote.
Compared to the control group without infection, there was increased risk of post-acute sequelae in all 10 organ systems—cardiovascular, mental, neurologic, coagulation and hematologic, pulmonary, gastrointestinal, kidney, metabolic and musculoskeletal in the first year and nine organ systems (except kidney disorders) in the second year, the researchers found. Disorders involving three organ systems—neurologic, pulmonary and gastrointestinal—exhibited increased risks even in the third year.
‘Eye-Opener’
The finding that new complications were emanating three years after infection was “a bit of an eye-opener,” said Al-Aly, director of the Clinical Epidemiology Center and chief of the Research and Education Service at the VA Saint Louis Health Care System.
“We went through thinking when you get over COVID, you get over it, and if you haven’t really gotten any complications from COVID in the first few months then you are out of the woods so to speak,” he said. “We thought there would be no long-term effects, that it would start anew in the second or third year.”
This new finding not only opens researchers’ eyes to the long-term effects of COVID-19 but raises the possibility that other acute viral infections may have long-term effects, as well.
“We have been in the COVID pandemic for the past four years, so it is more on our mind, but it is unlikely that COVID is really unique,” he said.
“Even myself, I used to think of acute infections as inconsequential,” he said. “You get infected, you get sick for a day or two, but you bounce back, and the infection doesn’t have long-term consequences. But I think we should have a newfound respect or appreciation for acute infections.”
Future research is needed to determine the long-term effects of other viral infections, Al-Aly said. But, for now, his group’s work will continue to focus on the long-term effects of COVID-19, a task that is made possible due to the health records available through the VA and the sheer number of people who have been affected.
“We are very, very, very intent on doing follow-up studies 3 years, 5 years or even a decade after acute illness to try to more completely understand the long-term trajectories of health and illness in people with SARS-CoV-2 infection,” he said.
- Cai, M., Xie, Y., Topol, E. J., & Al-Aly, Z. (2024). Three-year outcomes of post-acute sequelae of COVID-19. Nature Medicine, 10.1038/s41591-024-02987-8. Advance online publication. https://doi.org/10.1038/s41591-024-02987-8

