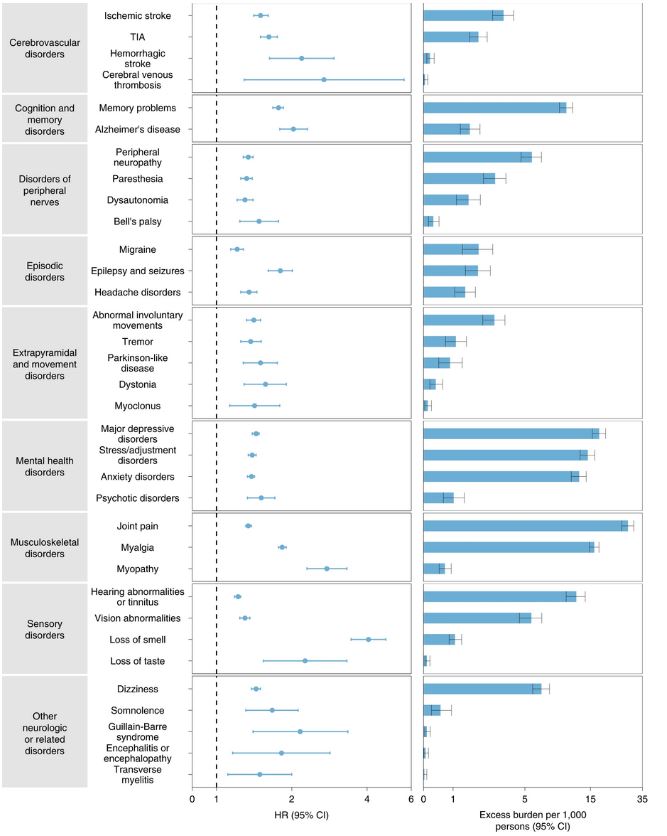
Click to Enlarge: Outcomes were ascertained 30 days after the COVID-19-positive test until the end of follow up. COVID-19 cohort (n = 154,068) and contemporary control cohort (n = 5,638,795). Adjusted HRs (dots) and 95% (error bars) CIs are presented, as are estimated excess burdens (bars) and 95% CIs (error bars). Burdens are presented per 1,000 persons at 12 months of follow up. The dashed line marks an HR of 1.00; lower limits of 95% CIs with values greater than 1.00 indicate significantly increased risk. Source: Nature Medicine
ST. LOUIS ― Patients face an increased risk of long-term neurologic conditions after suffering from COVID-19, including stroke, cognition and memory disorders, nervous system disorders, mental health disorders and more, according to a study examining the long-term effects of COVID-19.
The study published in Nature Medicine estimated the risks and burdens of incident neurologic disorders at 12 months following acute SARS-CoV-2 infection. The researchers used the VA’s national healthcare to build a cohort of 154,068 veterans who survived the first 30 days of COVID-19.
Their clinical outcomes were compared to two control groups of more than 11 million veterans who did not get COVID-19 (more than 5.6 million contemporary controls who use the VHA and nearly 5.9 million historical controls who used the VHA in 2017, which predates the COVID-19 pandemic.1
The longitudinal observational study focused on post-acute sequelae of COVID-19, also known as “long COVID,” which describe the long-term symptoms that might be experienced weeks to months after primary infection with SARS-CoV-2, according to the Centers for Disease Control and Prevention.
A comprehensive evaluation of post-acute COVID-19 clinical neurologic outcomes at 12 months was needed because previous studies were limited to people who were hospitalized during the acute phase of COVID-19. These studies had a follow-up duration of less than six months with a narrow selection of neurologic outcomes. Having information about post-acute COVID-19 neurologic outcomes at 12 months is critical to guiding post-acute COVID-19 care strategies and healthcare system capacity planning, according to the study.
The study’s main finding is that COVID-19 can lead to long-term neurologic disorders and that risk was evident even among those who had mild COVID-19, Ziyad Al-Aly, MD, chief of research and development at the St. Louis VA St. Louis Health Care System, told U.S. Medicine.
“We saw increased risk of neurologic problems in people with COVID; these included increased risk of strokes, cognitive impairment, headaches, seizures, inflammation of the brain, peripheral neuropathies, tingling and sensation problems, and several other disorders,” Al-Aly explained in an email.
In particular, patients were at greater risk of developing ischemic and hemorrhagic stroke, cognition and memory disorders, peripheral nervous system disorders, episodic disorders (e.g., migraine and seizures), extrapyramidal and movement disorders, mental health disorders, musculoskeletal disorders, sensory disorders, Guillain-Barré syndrome and encephalitis or encephalopathy, the study reported.
“Our study is the largest to date to comprehensively evaluate all the neurologic problems that can happen as a consequence of COVID-19,” Al-Aly wrote. “It is a detailed and comprehensive analysis of 44 outcomes using very large cohorts (more than 11 million people).”
Neurological Outcomes Widespread
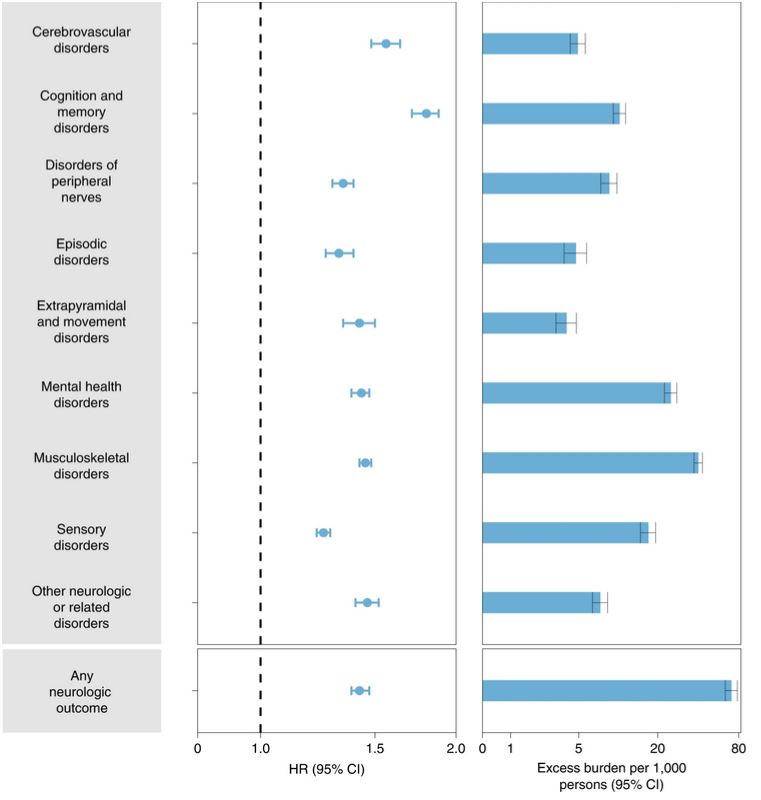
Click to Enlarge: Composite outcomes consisted of cerebrovascular disorders (ischemic stroke, TIA, hemorrhagic stroke and cerebral venous thrombosis), cognition and memory (memory problems and Alzheimer’s disease), disorders of the peripheral nerves (peripheral neuropathy, paresthesia, dysautonomia and Bell’s palsy), episodic disorders (migraine, epilepsy and seizures and headache disorders), extrapyramidal and movement disorders (abnormal involuntary movements, tremor, Parkinson-like disease, dystonia, myoclonus), mental health disorders (major depressive disorders, stress and adjustment disorders, anxiety disorders, and psychotic disorders), musculoskeletal disorders (joint pain, myalgia and myopathy), sensory disorders (hearing abnormalities or tinnitus, vision abnormalities, loss of smell and loss of taste), other neurologic or related disorders (dizziness, somnolence, Guillain–Barré syndrome, encephalitis or encephalopathy and transverse myelitis) and any neurologic outcome (incident occurrence of any neurologic outcome studied). Outcomes were ascertained 30 days after the COVID-19-positive test until the end of follow up. The COVID-19 cohort had n = 154,068 and the contemporary control cohort had n = 5,638,795. Adjusted HRs (dots) and 95% (error bars) CIs are presented, as are estimated excess burdens (bars) and 95% CIs (error bars). Burdens are presented per 1,000 persons at 12 months of follow up. The dashed line marks an HR of 1.00; lower limits of 95% CIs with values greater than 1.00 indicate significantly increased risk. Source: Nature Medicine
The risks of incident neurologic outcomes were evident in all subgroups based on age, race, sex, obesity, smoking, area deprivation index (ADI), diabetes, chronic kidney disease, hyperlipidemia, hypertension and immune dysfunction. Interaction analyses between age and exposure suggested that the risks of episodic disorders, mental health disorders, musculoskeletal disorders and any neurologic disorder increased as age increased. However, risks of cognition and memory disorders, sensory disorders and other neurologic or related disorders decreased as age increased.
The risks and burdens of the neurologic outcomes were evident even among those who were not hospitalized during the acute phase of COVID-19 and increased according to the severity of the acute infection from nonhospitalized to hospitalized to those admitted to intensive care. The findings were consistent in comparisons involving the contemporary control group and the historical control group, according to the study.
Limitations of the study include a cohort comprising mostly white males.
Health professionals and health systems caring for people who have had COVID-19, who are now the majority, are advised to care for patients with the understanding in mind that they’re at increased risk of developing neurologic problems. Providers need to help identify these neurologic issues and treat problems early on, Al-Aly wrote.
It’s important to understand that COVID-19 will likely have aftereffects that will persist for a lifetime, Al-Aly added.
“Because of the colossal scale of the pandemic, there will be millions of people bearing the scars of COVID for a lifetime,” Al-Aly explained. “These people will need care and this will invariably impact healthcare systems, costs and the economy. When the pandemic recedes from public view, we will be left with its after effects, which will reverberate with us for decades.”
The “risks and burdens of neurologic disorders in the COVID-19 group at 12 months are substantial,” the study reports. Given the massive scale of the COVID-19 pandemic, a large number of people around the world could be affected, contributing to a rise in the burden of neurologic diseases.
The study recommended that long-term consequences of SARS-CoV-2 infection should be taken into account when devising policies for managing the ongoing pandemic, and health systems should consider these findings in capacity planning and in designing clinical care pathways to address the needs of people who survive the acute phase of COVID-19.
- Xu E, Xie Y, Al-Aly Z. Long-term neurologic outcomes of COVID-19. Nat Med. 2022 Sep 22. doi: 10.1038/s41591-022-02001-z. Epub ahead of print. PMID: 36138154.


