Seattle, WA — Chronic obstructive pulmonary disease (COPD) is the sixth-most-common cause of death in the United States, but the link between medications and a greater risk of morbidity and mortality in those patients is not well known, according to a new report.
Falls frequently occur among COPD patients and often are associated with increased morbidity, mortality and healthcare costs. A better understanding of modifiable medication factors that contribute to fall risks could help with prevention strategies, the authors wrote.
That is of special concern to the VA, which provides care for approximately 500,000 patients with a diagnosis of COPD. The condition also is among the most common discharge diagnoses from VAMCs.
The retrospective cohort study used electronic health record data from a single health system linked to Washington state death certificates of COPD patients ages 40 or older who died between 2014-2018. Researchers led by Duke University School of Medicine identified demographics, comorbidities, fall-risk increasing drug (FRID) burden and the occurrence of injurious falls within the 2 years prior to the date of death. The VA Puget Sound Healthcare System and the University of Washington, both in Seattle, also participated in the study.
The results, published in the Journal of the COPD Foundation, noted that, of 8,204 decedents with COPD, 2,454 (30%) had an injurious fall in the 2 years before death, and FRID use was common among 65%.1
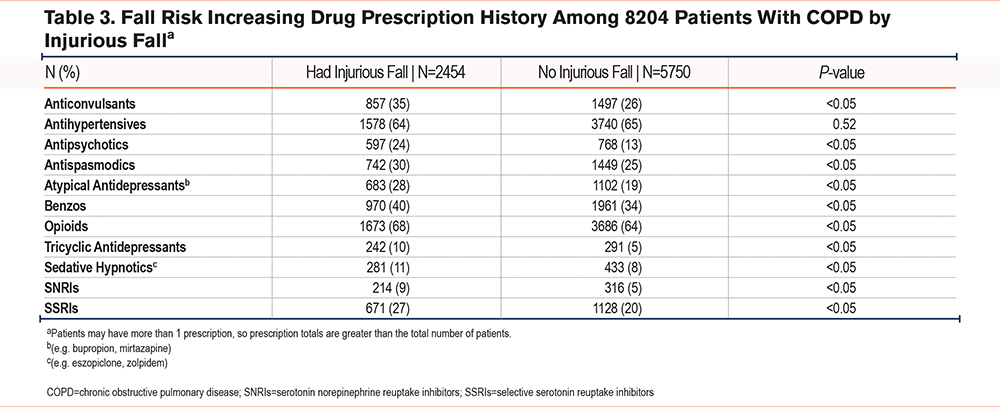
The study pointed out that a higher percentage of patients with falls received prescriptions for anticonvulsants (35% vs. 26%), antipsychotics (24% vs. 13%), atypical antidepressants (28% vs. 19%), tricyclic antidepressants (10% vs. 5%) versus those without a fall. The researchers added that, in multivariable logistic regression, after adjusting for confounders, FRID burden was associated with greater odds of injurious fall (odds ratio (OR) 1.07 (95% confidence interval (CI) 1.04-1.09).
“Our findings highlight an opportunity for collaboration between pharmacists, pulmonologists, and patients to develop new processes to potentially deprescribe and optimize the use of FRIDs among patients with COPD to increase safety,” the authors advised.
Causes of Falls
The causes of increased fall risk include frailty, impaired gait and tripping hazards from oxygen tubing, according to the report. “Despite COPD being the sixth most common cause of death in the United States, little is known about falls among these patients near the end of life,” the researchers added. “One modifiable risk factor for falls is medication use, including fall-risk increasing drugs (FRIDs) such as benzodiazepines, sedative-hypnotics, antihypertensives, and other psychoactive agents. Patients with COPD have a high prevalence of comorbidities for which FRIDs are often used as treatment, including anxiety, depression, diabetes, and hypertension.”
The study team suggested that the burden of polypharmacy also increases as patients’ function declines, and they receive additional medications for insomnia and pain, adding, “while these medications are intended to alleviate patient symptoms, they also increase the risk of injurious falls. Reducing FRID burden represents an opportunity to improve patient outcomes.”
They added that previous work has found an association between polypharmacy and increased fall risk, but that “FRID burden among patients with COPD, and the relationship between FRID burden and fall risk has not been previously described. FRID use among patients with COPD is of particular concern given the large number of FRID indications (e.g., anxiety, insomnia, dyspnea) among patients with COPD.”
The researchers pointed out that it can be difficult to decide which medications should be prioritized for dose reduction or discontinuation, adding, “We note that the most prescribed FRID class among all patients with COPD was antihypertensives. While the difference between the 2 groups with falls was not statistically significant, this still may be an area to consider deprescribing and/or dose reducing for patients with COPD, especially for those with episodes of orthostatic hypotension, well-controlled blood pressure, or limited life expectancy. In a previous study of older adults that explored ways to address medication-related symptoms, patients with COPD were more likely to prioritize reduction of fall injuries compared to reduction of cardiovascular events.”
They added that the second- and third-most-common FRID classes in their analysis were opioids and benzodiazepines. Often prescribed as palliation to relieve breathlessness or anxiety among patients with COPD, the authors noted that, “while such medications are appropriate in this context, additional fall mitigation options should be considered. We noted that patients with falls were more likely to receive anticonvulsants, antipsychotics, atypical antidepressants, tricyclic antidepressants, and SSRIs. These medications are often used for pain, insomnia, and depression; nonpharmacological options could perhaps reduce some medication use and thus, lower fall risk.”
The study also pointed to dementia as a more-common comorbidity among those with a fall compared with those who did not fall. “When possible, nonpharmacological alternatives to FRIDs, or using the lowest FRID dose possible for the shortest duration should be encouraged for patients living with both COPD and dementia,” the researchers recommended.
- McDermott CL, Feemster LC, Engelberg RA, Spece LJ, Donovan LM, Curtis JR. Fall Risk and Medication Use Near End of Life Among Adults With Chronic Obstructive Pulmonary Disease. Chronic Obstr Pulm Dis. 2024 Oct 25. doi: 10.15326/jcopdf.2024.0551. Epub ahead of print. PMID: 39480990.