VA Researchers Helped Lead Study on Overestimation of ASCVD Risk
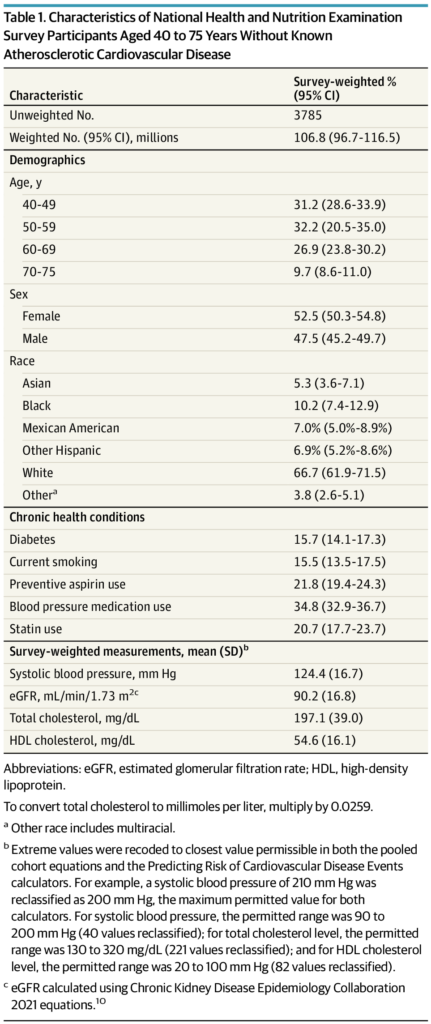
Click to Enlarge: Characteristics of National Health and Nutrition Examination Survey Participants Aged 40 to 75 Years Without Known Atherosclerotic Cardiovascular Disease. Source: JAMA Network Open
PITTSBURGH — Equations that estimate 10-year risk of atherosclerotic cardiovascular disease (ASCVD) appear to have overestimated the number of U.S. adults eligible for primary prevention statin therapy, according to a new study.
The research published in JAMA Internal Medicine sought to determine how estimates of 10-year atherosclerotic cardiovascular disease (ASCVD) risk and recommendations for primary prevention statin therapy differ between the 2023 American Heart Association (AHA) Predicting Risk of Cardiovascular Disease Events (PREVENT) equations and the 2013 AHA/American College of Cardiology pooled cohort equations (PCEs).1
The authors from the Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System and the University of Pittsburgh and their colleagues conducted a cross-sectional study of 3,785 adults aged 40 to 75 years without known ASCVD weighted to be representative of the U.S. population. They found that the use of the PREVENT equations was associated with reduced ASCVD risk estimates across age, sex and racial groups compared with the PCEs.
In fact, based on PREVENT equations, 17.3 million adults who were previously recommended to receive primary prevention statin therapy would no longer meet eligibility, including about 4.1 million adults currently taking the drugs. Others didn’t follow the recommendations and reported no use of statins.
The study team, including participation from the VA Ann Arbor, MI, Healthcare System, suggested that the use of the PREVENT equations could greatly reduce the number of patients eligible for primary prevention statin therapy.
In 2023, AHA developed the PREVENT equations to estimate 10-year risk of ASCVD as an update to the 2013 pooled cohort equations (PCEs). The PREVENT equations, which were derived from contemporary cohorts, removed race as a factor but added variables for kidney function and statin use.
Included in the study were participants in the National Health and Nutrition Examination Survey from 2017 to March 2020. Adults were defined as eligible for primary prevention statin use based on the 2019 AHA guidelines. The researchers weighted data to be nationally representative; analysis occurred from Dec. 27, 2023, to Jan. 31, 2024.
In the weighted sample of 52.5% of women and a mean age of 55.7 without known ASCVD, 20.7% reported current statin use. The study team calculated that the mean estimated 10-year ASCVD risk was 8.0% (95% CI, 7.6%-8.4%) using the PCEs and 4.3% (95% CI, 4.1%-4.5%) using the PREVENT equations.
“Across all age, sex, and racial subgroups, compared with the PCEs, the mean estimated 10-year ASCVD risk was lower using the PREVENT equations, with the largest difference for Black adults (10.9% [95% CI, 10.1%-11.7%] vs. 5.1% [95% CI 4.7%-5.4%]) and individuals aged 70 to 75 years (22.8% [95% CI, 21.6%-24.1%] vs. 10.2% [95% CI, 9.6%-10.8%]),” the authors advised. The use of the PREVENT equations instead of the PCEs could reduce the number of adults meeting criteria for primary prevention statin therapy from 45.4 million (95% CI, 40.3 million-50.4 million) to 28.3 million (95% CI, 25.2 million-31.4 million).
“In other words, 17.3 million (95% CI, 14.8 million-19.7 million) adults recommended statins based on the PCEs would no longer be recommended statins based on PREVENT equations, including 4.1 million (95% CI, 2.8 million-5.5 million) adults currently taking statins,” they added.
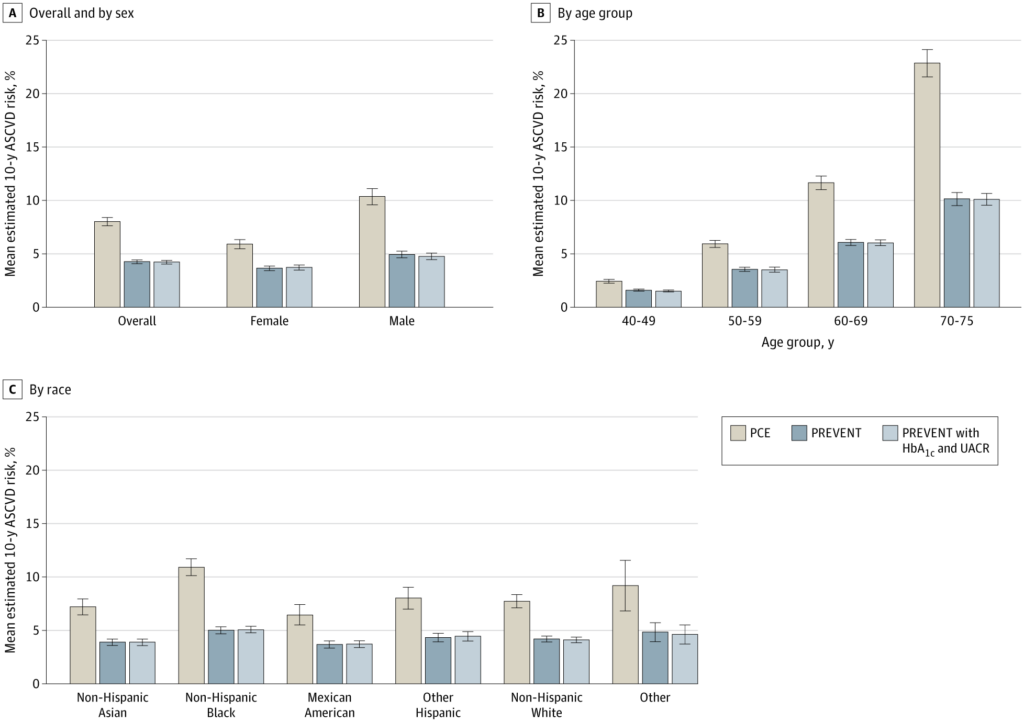
Click to Enlarge: Estimated Mean 10-Year Atherosclerotic Cardiovascular Disease (ASCVD) Risk, by Calculator Error bars, represent 95% CIs. Other race includes multiracial. HbA1c indicates hemoglobin A1c level; PCE, pooled cohort equation; PREVENT, Predicting Risk of Cardiovascular Disease Events; and UACR, urine albumin-to-creatinine ratio Source: JAMA Network Open
The study noted that, based on the PREVENT equations, 44.1% (95% CI, 38.6%-49.5%) of adults eligible for primary prevention statin therapy reported currently taking statins. That meant that 15.8 million (95% CI, 13.4 million-18.2 million) adults eligible for primary prevention statins reported that they were not taking them.
Overestimation Concerns
Background information in the article pointed out that concerns have been raised that the PCEs, which are derived from five cohorts initially recruited between the 1940s and 1980s, might “broadly overestimate” risk for current populations. Furthermore, critics have claimed that the cohorts underlying the calculation of the equations were not reflective of the current diversity of the U.S. population, with Asian and Hispanic adults especially underrepresented.
In 2023, the AHA Cardiovascular-Kidney-Metabolic Scientific Advisory Group developed and externally validated the Predicting Risk of Cardiovascular Disease (CVD) Events (PREVENT) equations. The new algorithms provided an alternative calculator for estimating 10-year ASCVD risk, as well as separate calculators for estimating heart failure and total cardiovascular risk.
“Compared with the PCEs, the PREVENT equations omit race and include measures of renal function and statin use as well as optional variables for hemoglobin A1c (HbA1c) level, the urinary albumin-to-creatinine ratio (UACR), and the social deprivation index,” the researchers explained. “The PREVENT equations were developed in part from more diverse and contemporary cohorts derived from electronic health record data.”
More than 50 million U.S. adults age 40 years and older meet criteria for elevated ASCVD risk and thus meet the recommendation for primary prevention statin use based on the current PCEs, they added, but it was not clear whether the PREVENT equations changed risk prediction or treatment recommendations compared with the PCEs or whether differences exist across demographic groups.
“While the current study focused on primary prevention statin therapy recommendations, ASCVD risk estimation plays a role in other aspects of current preventive cardiology practice,” according to the report. “Notably, current guidelines for blood pressure management recommend different treatment thresholds for patients with a 10-year ASCVD risk greater than 10%, and recommendations for primary prevention aspirin use are also based on ASCVD risk calculation. Thus, adoption and implementation of the PREVENT equations could substantially lower multiple domains of preventive medication use, particularly among older adults, which might reduce polypharmacy.
“This potential practice change has some parallels to shifts in the recommendations on aspirin use for primary prevention of ASCVD. However, deimplementing statins for the 4.1 million adults in the U.S. who would no longer meet ASCVD risk criteria but currently take statins could be more challenging, with the potential to lead to patient confusion over shifting recommendations, particularly as many adults at borderline risk of ASCVD may again reach statin eligibility after a few years. Changing risk estimation will also alter which patients are recommended to be evaluated for risk-enhancing factors, including lipoprotein(a) and coronary artery calcium screening.”
The authors also discussed policy implications, suggesting that “electronic health record-based cohorts that underlie key risk scores should be augmented with methods to assess and improve data accuracy and reduce bias,” adding, “Finally, the process of risk estimation is sufficiently uncertain and unstable that we should consider moving away from precise treatment thresholds toward recommendations that encourage risk communication and shared decision-making.”
- Anderson TS, Wilson LM, Sussman JB. Atherosclerotic Cardiovascular Disease Risk Estimates Using the Predicting Risk of Cardiovascular Disease Events Equations. JAMA Intern Med. Published online June 10, 2024. doi:10.1001/jamainternmed.2024.1302


