Issue Appears to Be Aggressively Managed Diabetes

Sebhat Erqou, MD, PhD, Cardiologist with the VA Providence Medical Center and Assistant Professor of Medicine, at the Alpert Medical School, Brown University
PROVIDENCE, RI — Optimal diabetes management requires striking a careful balance. Over time, high blood glucose levels impair cardiovascular function, leading to delayed wound healing, heart disease and elevated risk of stroke. On the flip side, low blood sugar levels can sometimes lead to falls, loss of consciousness, seizures and death.
A new study indicates hypoglycemia may also lead to a prolonged QT interval in patients with Type 2 diabetes. As QT prolongation increases, the risk of potentially fatal arrhythmias and sudden cardiovascular events, the finding by VA researchers and others may solve a long-standing mystery.
Fifteen years ago, the landmark Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial called into question the wisdom of interventions designed to achieve normal glycated hemoglobin levels in individuals with Type 2 diabetes at high risk of cardiovascular disease. Based on studies that showed a reduction in microvascular complications at lower HbA1c levels, the trial investigators expected that targeting an HbA1c of 6% or less would reduce mortality in this patient group compared to HbA1c of 7% to 7.9%.1
The trial instead revealed that the lower HbA1c target increased the risk of cardiovascular-related mortality by 35% and all-cause mortality by 22%. The increased mortality risk persisted for years after the study concluded. ACCORD also found that participants in the intensive therapy arm experienced more than three times the rate of severe hypoglycemia (SH). Other studies confirmed an association between SH and all-cause and cardiovascular mortality.2
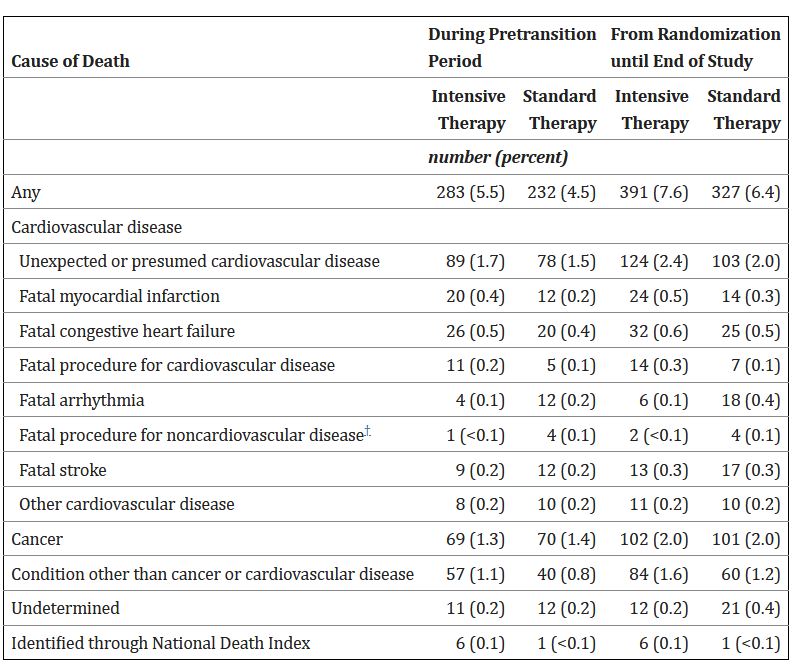
Click to Enlarge: *Data within categories are not mutually exclusive, and persons who were classified as having more than one possible cause of death are listed in the relevant categories.
†This condition was a component of the outcome of fatal cardiovascular disease. Source: New England Journal of Medicine. 2011 Mar 3; 364(9): 818–828.
Why hypoglycemia increases mortality risk in patients with Type 2 diabetes remained a puzzle, however. Researchers at the Providence, RI, VAMC and the VA Boston Healthcare System and others thought part of the answer could lie in a connection between severe hypoglycemia and prolonged QT interval. “The heart rate (HR) corrected QT (QTc) interval is a measure of myocardial repolarization that is positively associated with a higher risk of fatal ventricular arrhythmias,” wrote the researchers in a recent issue of The Journal of Clinical Endocrinology and Metabolism. Further, they noted that some smaller studies found a link between SH and prolonged QT interval. Did that explain the detrimental effects of intensive therapy in patients with Type 2 diabetes?3
Hypoglycemic Episodes
To find out, they conducted a prospective cohort analysis of the ACCORD study, that included 8,277 participants in the trial who had documented normal QTc at baseline and were not taking drugs associated with QTc prolongation. Participants were regularly queried about severe hypoglycemic episodes throughout the study and had 12-lead electrocardiograms (ECGs) at baseline, year two and at the exit interview. A prolonged QTc was defined as more than 460 ms in women and more than 450 ms in men.
During a five-year follow-up period, 517 participants developed incident prolonged QT interval. Of those, 481 cases occurred among 7,953 participants who did not experience severe hypoglycemia, a 6.1% rate. Among the 324 participants who experienced SH, the rate of prolonged QT was nearly doubled, at 11.1%.
“After multivariable adjustment, severe hypoglycemia was associated with elevated risk of incident QTc prolongation (RR 1.66, 95% CI 1.16-2.38, P=0.005). Adjustments for other QTc formulas did not affect the association,” the researchers noted. Compared with participants without severe hypoglycemia, those who had one hypoglycemia episode had a 57% increased relative risk, while those who had two or more episodes had double the relative risk. Participants younger than 61.9 years who had severe hypoglycemia had more than twice the relative risk of those who did not, while the difference among older participants was not significant.
“We observed that severe hypoglycemia with incident QTc prolongation in a large cohort of adults with Type 2 diabetes,” the authors concluded. “Moreover, we observed that this association was more profound among younger participants.”
The researchers posited four possible explanations for the connection between severe hypoglycemia and prolonged QT interval. The first is an effect on the human ether-ag-go-related gene potassium channel, which plays a central role in cardiac repolarization. Sympathoadrenal response is another possibility as is hypokalemia, which can profoundly affect myocardial cells, leading to arrhythmia. The last potential explanation was intracellular calcium oscillations that could also cause membrane depolarization.
Regardless of the precise mechanism, the authors noted that “our report complements prior experimental or small-scale clinical studies by providing data from a large prospective study that support the putative role of severe hypoglycemia in the development of QTc prolongation, a precursor to lethal ventricular tachyarrhythmias, in people with Type 2 diabetes.”
“The take-home message for clinicians would be to be cognizant of potential risks of arrhythmia with aggressive blood glucose control in particular in people who are already susceptible e.g., people on QT-prolonging medications, or people with cardiac dysfunction. In those cases, less ambitious blood glucose targets may be considered,” co-author Sebhat Erqou, MD, PhD, a cardiologist with the VA Providence Medical Center and assistant professor of medicine, at the Alpert Medical School, Brown University, told U.S. Medicine.
Lessons From the Study
Based on the findings from this study, the researchers made several recommendations for managing patients with Type 2 diabetes in clinical practice. “Our study points to the potential utility of a systematic assessment of QTc interval from a 12-lead ECG in the setting of an episode of severe hypoglycemia,” they said. In addition, in patients with Type 2 diabetes at high risk of hypoglycemia who have a history of QTc prolongation, continuous glucose monitors “could potentially prevent death.”
As a practical matter, the “focus should be mainly avoiding hypoglycemia in patients with diabetes, while trying to control their blood sugar,” Erqou added. “Studies have indicated that certain groups of people, especially older people, are more susceptible to adverse effects when aggressive blood glucose control strategies are implemented,”
“Particular attention may be paid to those patients who are concomitantly on medications that prolong their QT intervals,” Erqou said. “For example, some diabetic patients with diabetic GI complications (e.g., gastroparesis) may be chronically taking medications that promote gastric emptying such as metoclopramide, which are also QT prolonging.”
- Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008 Jun 12;358(24):2545-59. doi: 10.1056/NEJMoa0802743. Epub 2008 Jun 6. PMID: 18539917; PMCID: PMC4551392.
- ACCORD Study Group, Gerstein HC, Miller ME, Genuth S, Ismail-Beigi F, Buse JB, Goff DC Jr, Probstfield JL, Cushman WC, Ginsberg HN, Bigger JT, Grimm RH Jr, Byington RP, Rosenberg YD, Friedewald WT. Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med. 2011 Mar 3;364(9):818-28. doi: 10.1056/NEJMoa1006524. PMID: 21366473; PMCID: PMC4083508.
- Kaze AD, Yuyun MF, Erqou S, Fonarow GC, Echouffo-Tcheugui JB. Severe Hypoglycemia and Incidence of QT Interval Prolongation Among Adults with Type 2 Diabetes. J Clin Endocrinol Metab. 2022 Apr 9:dgac195. doi: 10.1210/clinem/dgac195. Epub ahead of print. PMID: 35396596.

