Favorably Affected Risk of Hospitalizations in Veteran Patients
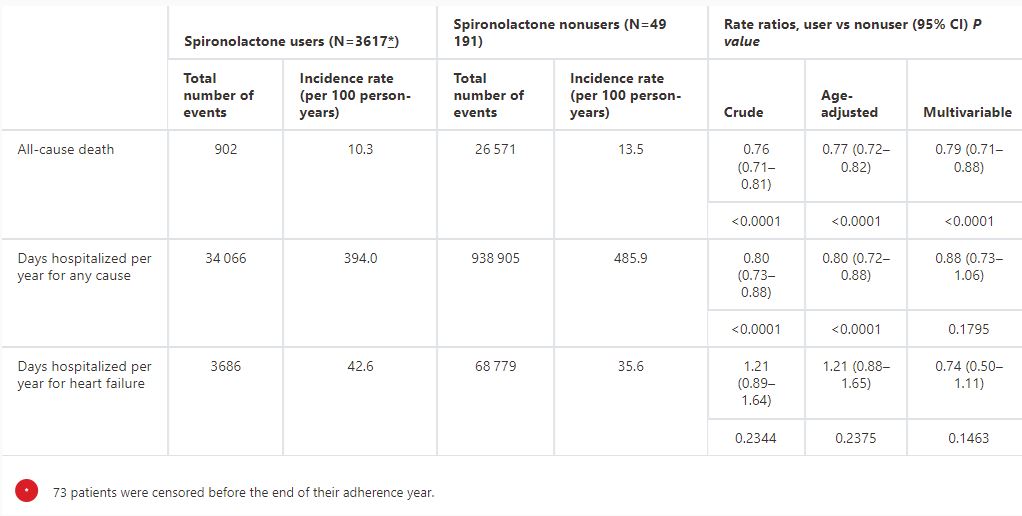
Click to Enlarge: Association of Spironolactone Use With Death and Hospitalizations, Censoring 60 Days After the End of the Last Prescription
Source: JAHA
BOSTON — For veterans with heart failure with preserved ejection fraction (HFpEF), spironolactone use reduced all-cause death and demonstrated a favorable trend in reducing hospitalizations, according to a study of a real-world national cohort of patients with HFpEF.
Increasing in prevalence and diagnosed in millions worldwide, HFpEF is a complex syndrome that sometimes can be difficult to manage because of a dearth of evidence-based therapies, according to the researchers from the Massachusetts Veterans Epidemiology and Research Information Center (MAVERIC) VA Boston Healthcare System and colleagues.
Based on previous research that suggested a benefit, the study team sought to determine the effectiveness of spironolactone in reducing death and hospitalization outcomes for patients with HFpEF in a real-world setting. Results were published in the Journal of the American Heart Association.1
Electronic health records from the VA healthcare system between 2002 and 2012 were used to identify patients with HFpEF who were followed longitudinally through 2014 using a validated algorithm. The researchers identified 2,690 spironolactone users and 49,191 nonusers among an HFpEF cohort that was 96% men, 85% white and with a median age of 74. The patients were followed for a median of 2.9 (interquartile range [IQR], 1.5-2.4) and 3.3 (IQR, 1.6-5.9) years, respectively.
The study team observed crude rates of 10.3 vs. 13.5 deaths and 394.0 vs. 485.9 days hospitalized were observed per 100 person-years for spironolactone users compared to nonusers, respectively. “After multivariable adjustment, there was a 21% reduction (95% CI, 13-29; P <0.0001) in rate of all-cause death among spironolactone users compared with nonusers and no statistically significant difference in days hospitalized for all causes or heart failure,” the authors reported, adding, “In a real-world national cohort of patients with HFpEF, spironolactone use reduced all-cause death and demonstrated a favorable trend in reducing the burden of hospitalizations.”
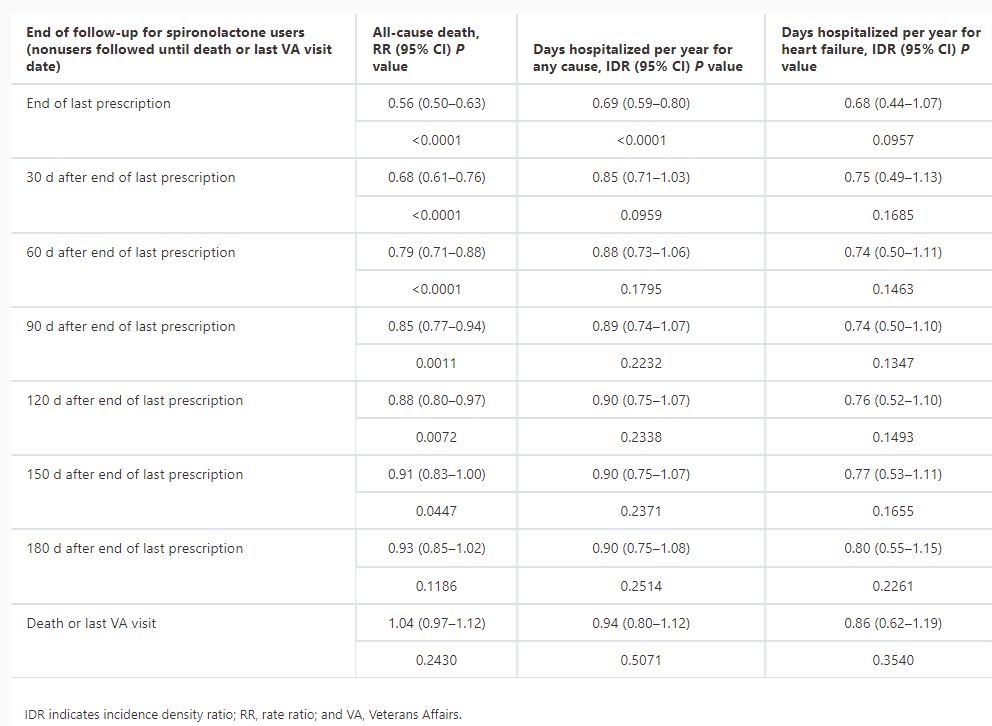
Click to Enlarge: Sensitivity Analyses: Association of Spironolactone Use With Death and Hospitalizations, Censoring at 30‐Day Increments After the End of the Last Prescription
Source: JAHA
The researchers recommended that mineralocorticoid antagonism should be strongly considered in patients with heart failure with preserved ejection fraction. They suggested that ongoing clinical trials will further elucidate the benefits of spironolactone in heart failure with preserved ejection fraction.
Background information in the article described how HFpEF makes up about half of the 6.2 million prevalent heart failure (HF) cases in the United States. “HFpEF is associated with poor quality of life, high morbidity and mortality rates, and high health care usage,” the authors explained. “The prevalence of HFpEF has been increasing, likely due to improved clinical recognition and increasing life expectancy among the aging population, The HFpEF epidemic is increasing at rates faster than other types of HF.”
They added that, recently, sodium glucose cotransporter 2 inhibitors were shown to reduce hospitalizations in HFpEF, which has a high rate of morbidity and mortality and angiotensin-neprilysin inhibition previously were found to benefit subsets of HFpEF.
The article pointed out that spironolactone is a potassium‐sparing diuretic and mineralocorticoid receptor antagonist, which has been used to treat a wide range of conditions including cirrhosis, nonalcoholic fatty liver disease, polycystic ovary syndrome, diabetic nephropathy and hypertension, adding that the RALES (Randomized Aldactone Evaluation Study) trial demonstrated that spironolactone is an effective treatment for HF with reduced ejection fraction.
“Given the success in HF with reduced ejection fraction and that spironolactone decreases the interstitial fibrotic process that is common in HFpEF, multiple clinical trials have investigated whether spironolactone also effectively treats HFpEF, with only a few that evaluated death and all‐cause hospitalization outcomes,” the researchers explained. “Though findings varied across studies, and many lacked significant results, meta‐analysis pooling data suggest that spironolactone improves diastolic function and reduces blood pressure in HFpEF but had minimal effect on death and hospitalization outcomes.”
The largest of those so far, TOPCAT (Treatment of Preserved Cardiac Function Heart Failure With an Aldosterone Antagonist Trial), also did not show a benefit on the primary composite outcome, although spironolactone did significantly reduce HF hospitalizations, they added.
More Trials on the Way
In addition, trial arms in the Americas showed significant outcome improvements with spironolactone, but that was not the case in areas such as Russia.
Additional trials, SPIRRIT‐HFPEF (Spironolactone Initiation Registry Randomized Interventional Trial in Heart Failure With Preserved Ejection Fraction) and SPIRIT‐HF (Spironolactone in the Treatment of Heart Failure), are currently underway to further assess the efficacy of spironolactone in HFpEF.
That led the researchers to investigate the effectiveness of spironolactone on death and hospitalization outcomes in a real‐world setting using national electronic health record data.
“In this large observational study using real‐world electronic health record data in a well‐curated national patient cohort with HFpEF, we demonstrate a significantly reduced mortality rate in HFpEF treated with spironolactone and extend the results of the TOPCAT study demonstrating benefit in a real‐world population,” they noted, adding, “Real‐world data can confirm the benefits observed in a clinical trial on a larger scale. For example, the largest meta‐analyses assessing death and hospitalization outcomes included no more than three trials and 2000 spironolactone users, while our study had 3690 HFpEF spironolactone users.”
One issue, the authors advised, is that the VA HFpEF cohort had less atrial fibrillation, chronic kidney disease, myocardial infarction, stroke and βblocker use than the TOPCAT Americas cohort, although the overall comorbidity burden of VA HFpEF cohort was likely similar to the TOPCAT Americas cohort due to the VA cohort having a higher proportion of individuals with diabetes (57% vs. 45%) and chronic obstructive pulmonary disease (50% vs. 16%).
The researchers also raised the issue that all HFpEF subphenotypes might not respond to a single therapy, and spironolactone may benefit only specific subgroups, explaining, “It is possible that there was less variation among HFpEF subphenotypes within our real‐world cohort, leading to less variability in outcomes and thus significant results in our study. Our HFpEF population is composed primarily of older white men with hypertension, diabetes, and dyslipidemia, which is analogous to the subphenotype described as having the highest risk of adverse outcomes.”
“We investigated the long‐term effectiveness of spironolactone use in a real‐world HFpEF population, without the restrictive inclusion and exclusion criteria of traditional clinical trials while maintaining stringent requirements for spironolactone exposure,” the study team concluded. “Our findings suggest that spironolactone improves survival in HFpEF. However, further investigation is necessary to determine if specific HFpEF subphenotypes might gain more benefit from spironolactone, especially over longer time periods.”
- Kurgansky KE, Parker R, Djousse L, Gagnon DR, Joseph J. Spironolactone Reduces the Risk of Death in Veterans With Heart Failure With Preserved Ejection Fraction. J Am Heart Assoc. 2024 Jul 16;13(14):e032231. doi: 10.1161/JAHA.123.032231. Epub 2024 Jul 9. PMID: 38979805.

