Click to Enlarge: Crude and Age-Adjusted Cardiac Disease Mortality Rates for US Women Veterans and Civilian Women Source: JAMA Network Open
LOS ANGELES — Women veterans have shown a lack of improvement in cardiac mortality compared to civilian women over nearly two decades, suggesting a need for clinical interventions to improve cardiovascular care, according to a recent study.
The retrospective longitudinal cohort study published in JAMA Network Open examined the trends for cardiac disease mortality for women veterans over the past two decades and compared them to rates for civilian women.1
Cardiovascular disease is “the leading cause of death in the United States, and women veterans have higher rates of cardiovascular disease compared to civilian women,” the authors explained. The researchers investigated recent trends in cardiac disease mortality among women veterans because few studies have explored this topic, the study reported.
The study authors were affiliated with the VA Greater Los Angeles Healthcare System in Los Angeles the VA North Texas Health Care System in Dallas; the Durham, NC, VAMC and the Northport, NY, VAMC.
The researchers analyzed VHA electronic health record data from the VHA Corporate Data Warehouse, linked with the National Death Index, to study cardiovascular disease trends and rates of cardiac disease mortality among 817,912 women veterans (18 years and older) who had used VHA healthcare facilities from Jan. 1, 2000, to Dec. 31, 2017. The data on women veterans were compared to a national cohort of civilian women (15 years and older) in the Centers for Disease Control and Prevention (CDC) Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database, which provides cause-of-death data using death certificates for all U.S. residents, according to the authors.
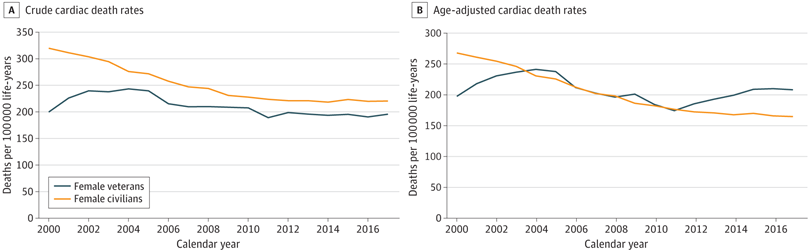
Crude and age-adjusted cardiac disease mortality rates (per 100,000 life-years), and 95% confidence intervals were calculated for women veterans and civilian women. The 2000 U.S. general population was the reference for age-adjusted rates, the researchers pointed out.
“During the study period, 2000 to 2017, there was no significant change in either the crude or the age-adjusted rates of cardiac mortality for women veterans,” Ramin Ebrahimi, MD, an interventional cardiologist and director of interventional cardiology research at VA Greater Los Angeles Healthcare System, told U.S. Medicine. “However, during the same time period, crude and age-adjusted rates of cardiac mortality decreased by 31% and 39% for civilian women, respectively. In 2017, the final year of the study, the age-adjusted rate of cardiac mortality was 26% higher for women veterans compared with civilian women.”
The authors determined that “19,022 cardiac disease deaths were identified among women veterans who engaged with VHA health care,” according to the study’s results. The investigation’s most-important finding is that “women veterans are at high risk for various cardiovascular diseases, including hypertension, heart disease, stroke and other circulatory disorders,” Ebrahimi wrote in an email.
“Our results provide some clarity for potential future directions for research and clinical interventions to improve cardiovascular health for U.S. women veterans,” said Ebrahimi, who is also a clinical professor of medicine at David Geffen School of Medicine at University of California, Los Angeles. He called the cohort an “at-risk population of U.S. veterans.”
The lack of reduction in cardiac disease mortality rate in women veterans occurred “despite changes in national guidelines that lowered the threshold for identification and treatment of cardiovascular disease risk factors, such as hypertension, hyperlipidemia, and diabetes,” according to the study.
Possible Explanations
Possible explanations for this lack of improvement in women veterans could be attributed to many factors, including “increasing rates of tobacco use, high treatment non-adherence rates, higher prevalence of cardiovascular risk factors that exceed rates for civilian women, greater overall clinical complexity, and the prevalence of nontraditional risk factors such as posttraumatic stress disorder, which is higher in women veterans,” the authors proposed.
Studies of U.S. women veterans are important because they are “the most diverse and fastest growing population of patients in the VA health care system,” Ebrahimi added. In the VHA, “women veterans are more diverse in terms of race and ethnicity compared with their men veteran counterparts,” the study pointed out.
Healthcare professionals who are treating women patients with cardiac disease need to understand that “sex differences exist in symptomatology, pathophysiology and treatment of cardiovascular disease, especially ischemic heart disease,” Ebrahimi recommended, adding, “Understanding such differences is important in providing better care to women with cardiovascular disease.”
The researchers haven’t formally analyzed the results based on race and ethnicity, but “preliminary results suggest potential race and ethnicity differences for cardiac mortality among U.S. women veterans,” Ebrahimi pointed out.
Ebrahimi noted this study investigated “difference in cardiac mortality as opposed to cardiovascular disease/circulatory mortality that also includes death as a result of hypertension, stroke or other circulatory disorders.”
“Our results should not be generalized to cardiovascular/circulatory deaths,” Ebrahimi said.
Because U.S. women veterans are an at-risk population, VA is working to increase awareness of heart disease in females and to enhance provider educational opportunities, according to the authors. The VA Office of Women’s Health “recognizes cardiovascular disease as the number one killer of women and that women veterans are at higher risk than women in the general population,” they explained.
In 2022, the VA Office of Women’s Health and the National Cardiology Program Office convened an interdisciplinary workgroup to develop dashboards and pilot protocols to reduce gender disparities in evidence-based treatment of cardiovascular disease. Also, the VA Office of Women’s Health has a memorandum of agreement with the American Heart Association to raise awareness of heart disease and stroke in women veterans, study authors pointed out.
In addition, the VA Office of Women’s Health is collaborating with researchers to develop the third edition of the “State of Cardiovascular Health in Women Veterans,” a report on the prevalence of cardiovascular disease and cardiovascular disease risk factors among women veterans, the study team added.
- Ebrahimi R, Yano EM, Alvarez CA, Dennis PA, Shroyer AL, Beckham JC, Sumner JA. Trends in Cardiovascular Disease Mortality in US Women Veterans vs Civilians. JAMA Netw Open. 2023 Oct 2;6(10):e2340242. doi: 10.1001/jamanetworkopen.2023.40242. PMID: 37902755; PMCID: PMC10616720.


