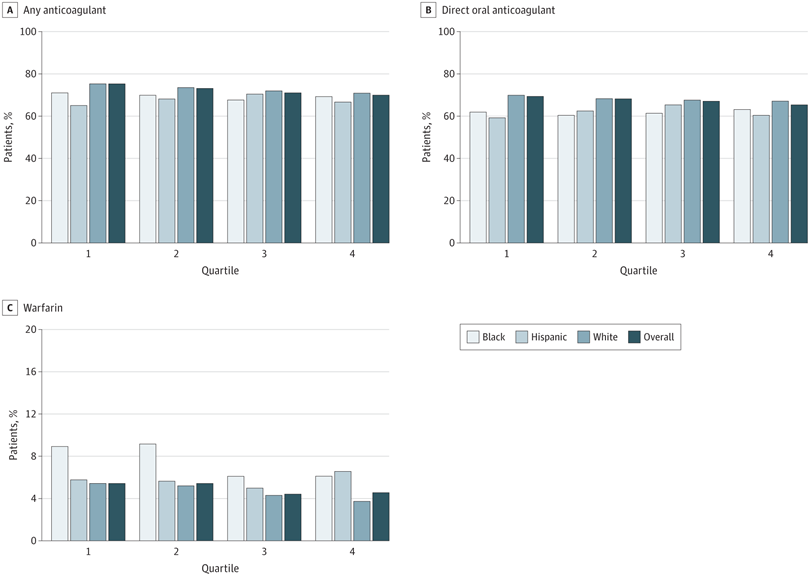
Click to Enlarge: A, The unadjusted rates of any oral anticoagulant therapy; B, direct oral anticoagulant therapy; and C, warfarin therapy initiation are displayed across quartiles (Q) of VA medical center racial and ethnic composition, overall and by race and ethnicity (Black, Hispanic, and White). Q1 represents VA medical centers with the lowest proportion of patients from minoritized racial and ethnic groups, and Q4 represents VA medical centers with the highest proportion of minoritized patients. Source: JAMA Network Open
LOS ANGELES — VA patients receive different medical care for atrial fibrillation depending on whether they visit a VAMC serving more minority patients, according to a new study.
The study published in JAMA Network Open reported that a national cohort of VA patients with atrial fibrillation who received care at minority-serving VAMCs were significantly less likely to receive any anticoagulant and warfarin therapy. No significant differences in the initiation of direct oral anticoagulant therapy were found at VAMCs serving fewer minority patients, however, the authors explained.1
Atrial fibrillation is the “most common heart rhythm problem in the United States, affecting about 6 million people. Previous studies have shown significant inequalities in atrial fibrillation treatment, especially with stroke-preventing medications,” study authors pointed out.
This retrospective cohort study investigated whether there’s an association between facility racial and ethnic composition and anticoagulant initiation among patients with atrial fibrillation treated in the VHA. The researchers wanted to explore this topic because “racial and ethnic disparities exist in anticoagulation therapy for atrial fibrillation, and it was unclear whether medical center racial and ethnic composition is associated with these disparities.” They suggested the “VA is an ideal place to study these treatment disparities because medication costs, which often prevent proper treatment, are not an issue.”
Study authors are affiliated with the Greater Los Angeles and Pittsburgh VA Healthcare Systems.
The cohort study involved 89,791 Black, white and Hispanic VA patients with atrial fibrillation from 2018 to 2021 at 140 VAMCs. VAMC racial and ethnic composition, which is defined as the proportion of patients from minoritized racial and ethnic groups treated at a VAMC, was categorized into quartiles. VAMCs in quartile 1 (Q1) had the lowest percentage of patients from minoritized groups. Data were analyzed from March to November 2023.
“Our study examined nearly 90,000 veterans with AFib from 2018 to 2021,” said lead author Utibe R. Essien, MD, MPH, of the VA Health Systems Research Center for the Study of Healthcare Innovation, Implementation and Policy in Los Angeles. “We discovered those VA medical centers with more veterans who were a racial or ethnic minority were much less likely to prescribe the recommended blood-thinning medications to prevent strokes in AFib patients.”
“The racial and ethnic disparities in anticoagulant prescribing means, as healthcare professionals who interact and treat these individuals, we should be conscious of the potential barriers that might lead to differential treatment for patients from minority groups,” Essien told U.S. Medicine. “We must continue to improve access to AFib care for all veterans.”
The findings suggested that “interventions to improve anticoagulant prescribing at minority-serving facilities may improve quality and equity of atrial fibrillation care in the VA.”
Participants in the study had a mean age of 73.0 years, and 87,647 (97.6%) were male. Also, 9,063 patients (10.1%) were Black, 3,355 (3.7%) were Hispanic, and 77,373 (86.2%) were white.
Lower rates of Anticoagulant Initiation
Among the participants, the authors found that “64,770 (72.1%) initiated any anticoagulant, 60,362 (67.2%) initiated direct oral anticoagulant (DOAC) therapy, and 4,408 (4.9%) initiated warfarin. Compared with white patients, Black and Hispanic patients had lower rates of any anticoagulant and DOAC therapy initiation, but higher rates of warfarin initiation across all quartiles of VAMC racial and ethnic composition.”
The authors also discovered that “any anticoagulant therapy initiation was lower in Q4 than Q1 (69.8% vs. 74.9%; adjusted odds ratio [aOR], 0.80; 95% CI, 0.69-0.92; P < .001). DOAC and warfarin initiation were also lower in Q4 than in Q1 (DOAC, 69.4% vs. 65.3%; aOR, 0.85; 95% CI, 0.74-0.97; P < .001; warfarin, 5.4% vs. 4.5%; aOR, 0.82; 95% CI, 0.67-1.00; P < .001).”
In addition, the study determined that “in adjusted models, patients in Q4 were significantly less likely to initiate any anticoagulant therapy than those in Q1 (aOR, 0.88; 95% CI, 0.78-0.99). Patients in Q3 (aOR, 0.75; 95% CI, 0.60-0.93) and Q4 (aOR, 0.69; 95% CI, 0.55-0.87) were significantly less likely to initiate warfarin therapy than those in Q1. There was no significant difference in the adjusted odds of initiating DOAC therapy across racial and ethnic composition quartiles.”
For healthcare professionals who are treating veteran patients with atrial fibrillation, it’s “key to understand prescribing inequities and who they affect. By educating themselves on why these inequities occur and reviewing their previous anticoagulant prescriptions to AFib patients, this can help healthcare professionals better understand if they, their practice or their VAMC can make changes to help improve equal access to AFib treatment for all veterans,” Essien explained.
In their research on pharmacoequity, the authors “aim to ensure all patients have access to life-saving medications regardless of race or social class,” the VA spokesperson said.
To manage this treatment issue, Essien noted that it’s important to “consider the ABCs, which are access, bias and cost.”
“By improving access, eliminating treatment bias, and reducing costs for patients, we can improve equity in treating AFib and address other medical disparities within the VA healthcare system,” he said. “This is an area that needs further study to find the reasons behind these disparities and overcome them.”
- Essien UR, Kim N, Hausmann LRM, Washington DL, Mor MK, Litam TMA, Boyer TL, Gellad WF, Fine MJ. Veterans Affairs Medical Center Racial and Ethnic Composition and Initiation of Anticoagulation for Atrial Fibrillation. JAMA Netw Open. 2024 Jun 3;7(6):e2418114. doi: 10.1001/jamanetworkopen.2024.18114. PMID: 38913375; PMCID: PMC11197447.

