Postoperative VTE rate was 1.3%
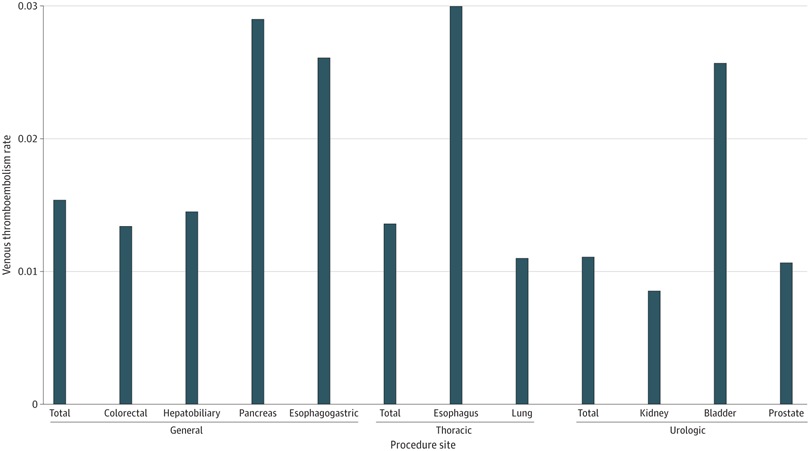
Click to Enlarge: The figure shows rates of venous thromboembolism by surgical specialty (general, thoracic, and urology) and procedure site. Overall rates of VTE were highest for patients who underwent esophagus, bladder, and pancreas procedures (P < .001). Source: JAMA Network Open
CHICAGO — The rates of venous thromboembolism (VTE) diagnosis are low after major cancer surgery among veterans treated at the VHA, according to a recent study.
The retrospective cohort study published in JAMA Network Open determined VTE rates after cancer surgery, in addition to rates of inpatient and outpatient (posthospital discharge) chemoprophylaxis adherence within the VHA, study authors reported.1
VTE, which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is a condition that occurs when a blood clot forms in a vein. It is highest after major surgery, major injury or during periods of infection and inflammation, according to the National Heart, Lung and Blood Institute. Chemoprophylaxis is the administration of a medication for the purpose of preventing disease or infection, the National Institutes of Health explained.
“Venous thromboembolism represents a major source of preventable morbidity and mortality and is a leading cause of death in the U.S. after cancer surgery,” David Bentrem, MD, professor of surgery and medical social sciences at Northwestern University Feinberg School of Medicine in Chicago and a researcher at Jesse Brown VAMC in Chicago told U.S. Medicine. “Previous research outside VHA demonstrated variability in venous thromboembolism chemoprophylaxis prescribing, though it is unknown how these rates compare with performance in VA.”
In the study, 30,039 veterans were surgically treated for cancer. The participants, who were 41 years or older without preexisting bleeding disorders or anticoagulation usage, underwent major abdominopelvic or thoracic surgery for cancer at a VA hospital between Jan. 1, 2015, and Dec. 31, 2022. Eligible patients were identified through the VHA Corporate Data Warehouse, Pharmacy Benefits Management database and VA Surgical Quality Improvement Program database. The analysis evaluated rates of postoperative VTE events within 30 days of surgery and VTE chemoprophylaxis adherence, according to the authors.
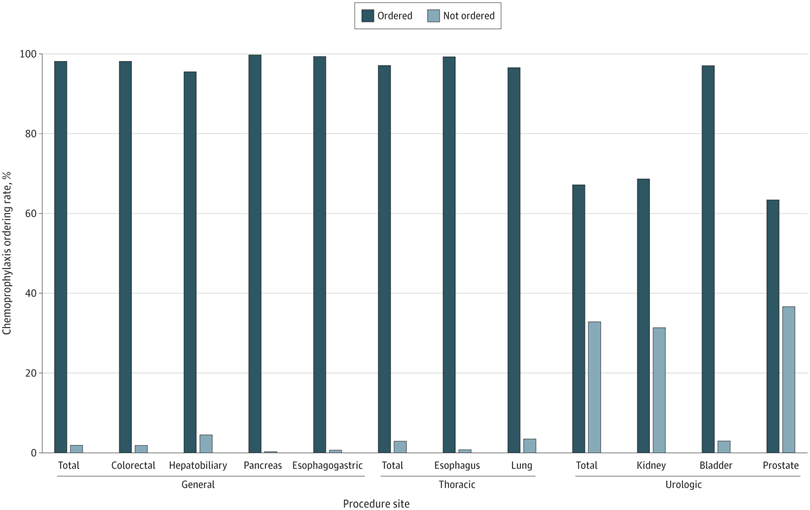
Click to Enlarge: The figure shows inpatient venous thromboembolism chemoprophylaxis ordering rates by surgical specialty (general, thoracic, and urology) and procedure site. Source: JAMA Network Open
The researchers were affiliated with Jesse Brown VAMC and the VA Health Services Research and Development Service and the Hines VAMC, all in Chicago, as well as the William S. Middleton VAMC in Madison, WI.
“In this retrospective cohort study, including 12,898 veterans surgically treated for cancer with Caprini score >5, venous thromboembolism rates were low (1.3%) despite variations in chemoprophylaxis ordering rates by surgical specialty and procedure site,” Bentrem said. “Specialty and procedure site variation exists for chemoprophylaxis and may be justified given low risks of overall and post-discharge venous thromboembolism.”
“The overall venous thromboembolism rate after major cancer surgery within the VA is low,” he added. “This is the first study to show VA inpatient chemoprophylaxis administration rates are high, and post-discharge venous thromboembolism chemoprophylaxis prescribing is similar to other large, non-VA health systems.”
Post-Discharge Chemoprophylaxis
The study found the “overall postoperative VTE rate was 1.3%, with 0.7% occurring during inpatient hospitalization and 0.6% occurring post-discharge. Inpatient chemoprophylaxis was ordered for 80.4% of patients, and the ordering rates were highest for general surgery (98.1%) and lowest for urology (67.1%) (p<0.001). Overall, 10.5% of patients received post-discharge chemoprophylaxis, with notable variation by specialty,” Bentrem explained.
Given the lower risk of VTE and prescribing habits similar to non-VA hospitals, the authors suggest that healthcare professionals should “assess each patient for their individual risk factors when prescribing outpatient chemoprophylaxis after major cancer surgery.”
The researchers pointed out that “patients who underwent urological procedures of the kidney and prostate were significantly less likely to receive inpatient VTE chemoprophylaxis compared with those who underwent any type of operation with general or thoracic surgery.” Patients who underwent prostate and kidney surgeries had the lowest rates of inpatient VTE chemoprophylaxis, but “rates of chemoprophylaxis for patients who underwent bladder operations were comparable to those for patients who underwent procedures with other specialties, and also had the highest rates of outpatient VTE chemoprophylaxis prescribing,” they added.
The variation is “likely due to the preference of practitioners and the perceived risk of bleeding after specific urological procedures balanced with the risk of VTE,” the study authors suggested.
Practitioners are likely assessing the risks appropriately, since “overall national VTE rates for patients undergoing urological procedures of the kidney and prostate were 0.9% and 1.1%, respectively,” the authors explained.
It’s less common to use VTE chemoprophylaxis based on risk, with exceptions including the “use of aspirin for chemoprophylaxis after orthopedic procedures and risk calculation to determine the need for extended postdischarge VTE chemoprophylaxis after bariatric surgery,” according to the authors. The study authors recommend that “risk-based de-escalation may be warranted for certain urological operations, particularly those involving the prostate or kidney, that have short lengths of hospital stay and high utilization of minimally invasive surgery.” The analysis also supports the development of “VTE risk calculators that are specific to both population and procedure site to guide chemoprophylaxis use,” the authors explained.
Limitations of this study include a population of mostly older men, which limits the generalizability of the research. Also, outpatient VTE chemoprophylaxis rates of self-administration were unclear, and there was no documentation of reported or measured patient home administration, the researchers pointed out.
- Logan CD, Hudnall MT, Schlick CJR, French DD, et. al. Thromboembolism Chemoprophylaxis Adherence Rates After Major Cancer Surgery. JAMA Netw Open. 2023 Sep 5;6(9):e2335311. doi: 10.1001/jamanetworkopen.2023.35311. PMID: 37768664; PMCID: PMC10539988.

