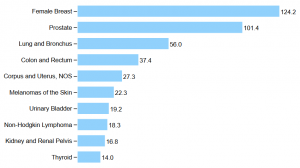
United States, 2016, Top 10 Cancers by Rates of New Cancer Cases: Male and Female
Rate per 100,000 people
WASHINGTON — The VA has adopted aggressive goals and a new national structure to bring precision medicine to the 15,000 veterans diagnosed each year with prostate cancer.
“We are building a state of the art oncology program so that veterans with prostate cancer can receive care in the VA equivalent to that in the nation’s leading cancers, regardless of their location,” said Kenute Myrie, PhD, scientific program manager of oncology, VA Office of Research and Development.
Prostate cancer is the most common malignancy among veterans, accounting for nearly 1 in 3 cases of cancer. It is a presumptive condition for veterans exposed to Agent Orange during their military service. More than 200,000 veterans are prostate cancer survivors.
The new initiative in precision oncology builds on the partnership established with the Prostate Cancer Foundation in 2016 as part of the National Cancer Moonshot launched by former Vice President Joe Biden. The PCF contributed an initial $50 million toward the initiative, followed in 2018 with $2.5 million from the John and Daria Barry Foundation to the PCF for the establishment of a center of excellence in the Manhattan campus of the VA NY Harbor Healthcare System.
The PCF partnership aimed to increase the number of prostate cancer researchers and studies at the VA, boost the number of VA facilities and veterans participating in prostate cancer-related precision medicine and clinical trials, and expand access to the wealth of anonymized patient data available through the VA to deepen understanding of impact of individual genetic variability on the occurrence, progression and treatment of cancer.
In addition, the PCF-VA partnership established increasing the number of minorities enrolled in PCF studies as a primary goal. African Americans are 64% more likely to develop prostate cancer and more than twice as likely to die from the disease than other men, according to the PCF. Prostate cancer represents more than 40% of all diagnosed cancers in African American veterans compared to 26% of cancers in their white former comrades-in-arms.1
“One of the unique things about the VA is the patient population,” Myrie told U.S. Medicine. “We have one of the highest concentrations of African Americans in a large, integrated healthcare system. African Americans are disproportionately affected by prostate cancer, yet in most clinical trials, the number of African Americans forms a very low percentage of participants. Increasing enrolment in trials at the VA will be very meaningful for the community, particularly as African-Americans have a more heterogenous genetic background than whites in most trials.”
Continue Reading:


Very inspiring article for PCa patients and providers. The precision treatment plan’s and genetic profiling’s effect on decision making will take a while but will probably give us a “leg up’ on the PCa
progression. To better use current and newer surgeries, radiation therapies and precision meds, earlier and more specifically.