However, Older Patients Have Not Benefited As Much
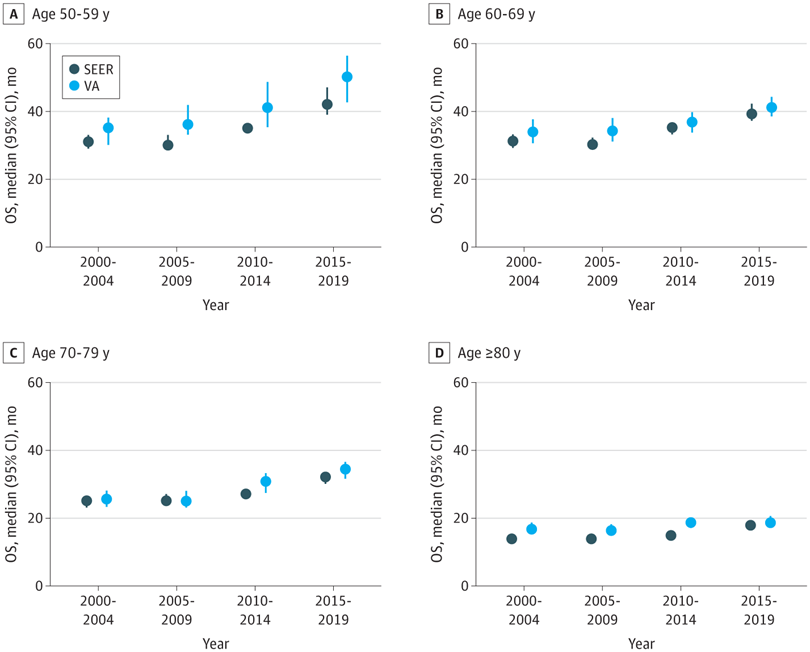
Click to Enlarge: Median Overall Survival (OS) of De Novo Metastatic Prostate Cancer in the Surveillance, Epidemiology, and End Results 17 (SEER) and Veterans Health Administration (VHA) Registries. The figure shows median survival by year of diagnosis, stratified by age at diagnosis of de novo metastatic prostate cancer in SEER and VHA registries. Error bars represent 95% CIs of the median. Source: JAMA Network Open
ST. LOUIS — Improved treatment has meant better overall survival for many men diagnosed with prostate cancer, according to a new research letter. For older patients, however, the benefits of the new therapies weren’t as effective, the authors pointed out.
“Overall survival (OS) in metastatic hormone-sensitive prostate cancer (mHSPC) has improved in clinical trials over the last 20 years,” wrote researchers from the Saint Louis VAMC and colleagues. “It is unclear whether new treatments have translated to improvements in survival rates in clinical practice.”
A report in JAMA Network Open described how the study team sought to quantify trends in OS among patients with newly diagnosed de novo (synchronous) metastatic hormone-sensitive prostate cancer (MHSPC) in two national registries in the United States: the Surveillance, Epidemiology, and End Results 17 (SEER) registry database and the VHA registry database.
Included in the study were patients diagnosed from 2000 to 2019 if the stage at first diagnosis of prostate cancer was distant metastasis from the SEER or VHA Oncology registry. Patients in VHA were observed until death or April 2022.
Of the study group, 58,859 patients were from SEER (median [IQR] age, 72 [64-81] years) and 14,904 patients from the VHA (median [IQR] age, 73 [65-81] years).
“From the years 2000 to 2004 to the years 2015 to 2019, median OS increased from 23.0 to 30.0 months in SEER (hazard ratio [HR], 0.80 [95% CI, 0.77-0.82]); median OS increased from 25.6 to 30.9 months in VHA (HR, 0.91 [95% CI, 0.87-0.96]),” according to the report in JAMA Network Open.1
While, among patients younger than 70 years, median OS increased from 31.0 to 40.0 months (HR, 0.78 [95% CI, 0.74-0.82]) in SEER and 34.3 to 42.2 months (HR, 0.87 [95% CI, 0.80-0.95]) in VHA, rates of better survival declined with age.
“Among patients aged 70 years or older, increases were more modest; from 19.0 to 24.0 months in SEER (HR, 0.83 [95% CI, 0.80-0.86]) and from 21.6 to 25.6 months in VHA (HR, 0.94 [95% CI, 0.88-1.00]),” the authors pointed out.
Half of Veterans Older Than 65
That is an issue for the VHA, because half of veterans are 65 and older. Prostate cancer is the most commonly diagnosed cancer among U.S. veterans, making up 30% of new cancer diagnoses in the VA healthcare system.
Many factors fuel the high rate of prostate cancer among patients who receive care through the VA, according to another study. Among them is that prostate cancer prevalence increases with age—with 50% to 60% of men over age 80 having indicative tumors on autopsy—and that VA patients are much more likely to be older and male than those in community healthcare systems. Another key reason is that prostate cancer is a presumptive condition for veterans exposed to Agent Orange.2
The new cross-sectional study found that median OS in de novo mHSPC was similar in SEER and VHA and had improved significantly in the U.S. population from 2000 to 2019, especially in patients younger than 70. “The improvements in OS mirror those observed in other countries and are likely due to the increased use of combination therapy,” the authors explained. “Our results suggest that new treatment paradigms may contribute to longer OS in clinical practice, which is the ideal setting to measure improvements in outcomes as treatments change.”
The study added that improved OS from trials cannot be assumed to reflect improvements in disease management in clinical practice. The researchers pointed out that the OS of men with mHSPC is lower in clinical practice than in clinical trials because patients are typically older with more comorbidities. In addition, they noted, trials that test similar clinical scenarios can produce drastically disparate OS.
“Our results highlight the poor OS in patients over 80 years of age, with little improvement over time,” according to the report. “This finding emphasizes the need to understand toxic effects vs. benefits and competing risks for mortality in older patients. Older patients with comorbid disease may not benefit from new therapies and may have higher risk of adverse events. Tailoring treatment for mHSPC based on comorbidities or genetic features may improve patient outcomes.”
The authors said their study was limited by lack of comorbidity data and that, because it was observational, causality cannot be determined.
“With improved detection of mHSPC, we expect that more patients will be determined to have mHSPC at diagnosis with smaller burden of disease and with longer survival due to stage migration rather than from improvements in treatment,” the researchers concluded. “Separating the effects of treatment from the effects of earlier mHSPC diagnosis will be more complex in the future.”
- Schoen MW, Montgomery RB, Owens L, Khan S, Sanfilippo KM, Etzioni RB. Survival in Patients With De Novo Metastatic Prostate Cancer. JAMA Netw Open. 2024;7(3):e241970. doi:10.1001/jamanetworkopen.2024.1970
- Shelton JB, Lynch J, Alba P, Anglin-Foot T, et. Al. Establishing a Prostate Cancer Data Core in VHA: Early Results. Presented at the Prostate Cancer Foundation 26th Annual Scientific Retreat. Oct. 24-26, 2019. Carlsbad, California.

