Study Suggests Levels Are Often Misinterpreted
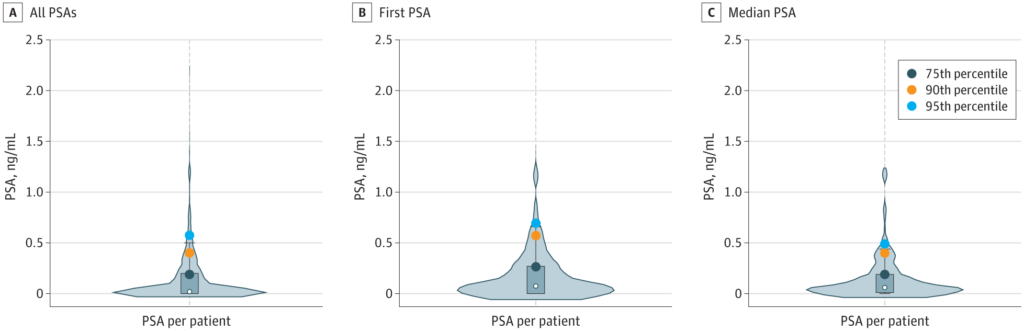
Click to Enlarge: Violin Plots of Prostate-Specific Antigen (PSA) Obtained per PatientA, All PSAs obtained (N = 852) in 210 patients meeting inclusion criteria. B, First PSA per patient, regardless of age. C, Median of all PSAs per patient. The rectangular shaded area on each plot represents the IQR and the white dot represents the median. Distribution of PSA values in transgender women receiving gender-affirming hormones is based on PSAs after estrogen use for at least 6 consecutive months. Source: JAMA Network Open
DURHAM, NC — In a VHA population, prostate-specific antigen (PSA) values in more than one-third of transgender women receiving estrogen were found to be undetectable, which indicates that PSA values in transgender women should be interpreted cautiously, according to a recent study.
The study published in JAMA “determined PSA values among a nationwide cohort of transgender women without known prostate cancer who are receiving estrogen, the most common gender-affirming hormone,” the authors reported. Study authors are affiliated with the VA Health Care System in Durham, NC.1
In individuals with prostate cancer, “transgender women receiving estrogen are more likely to present with high-grade disease versus cisgender men, which suggests potential delayed diagnosis. A likely reason for delayed diagnosis could be the absence of PSA reference ranges specific to transgender women receiving gender-affirming hormones. PSA, which is androgen-regulated, is expected to be lowered because of gender-affirming hormones,” the researchers explained.
In this study, the authors searched VHA records between January 2000 and August 2023 for adults with one or more diagnostic codes determined to be specific for transgender identity. The analysis identified 14,915 patients, and a detailed chart review of 1,000 randomly selected patients age 40 years or older was performed to establish the study cohort. “To be included in the study, patients had a confirmed identity as a transgender woman, no prostate cancer diagnosis, were receiving estrogen (regardless of orchiectomy status/other gender-affirming hormone usage), and a PSA test performed between the ages of 40 and 80 years old while receiving estrogen for six or more consecutive months”, study authors pointed out.
The researchers calculated PSA percentiles using all PSAs. Undetectable PSAs, meaning values below the lower limit of assay detection, were assigned a value of 0 ng/mL. The limited number of non-White patients prevented analyses by race. The analyses assessed PSA distributions using only one PSA per patient: the first PSA regardless of age and then the median of all PSAs per patient, the study reported.
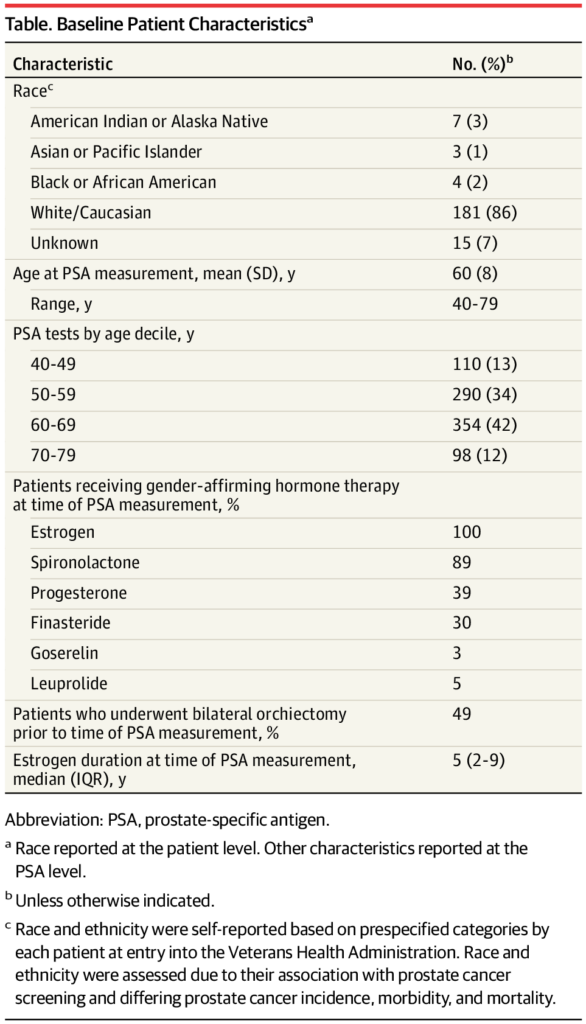
Click to Enlarge: Baseline Patient CharacteristicsaAbbreviation: PSA, prostate-specific antigen.
a. Race reported at the patient level. Other characteristics reported at the PSA level.
b. Unless otherwise indicated.
c. Race and ethnicity were self-reported based on prespecified categories by each patient at entry into the Veterans Health Administration. Race and ethnicity were assessed due to their association with prostate cancer screening and differing prostate cancer incidence, morbidity, and mortality. Source: JAMA Network Open
“The study found that the median PSA in transgender women receiving estrogen was 0.02 ng/mL, and the PSA level was undetectable in 36% of these patients,” co-author Amanda Hoedt, MS, of the VA Healthcare System in Durham, NC, told U.S. Medicine. “Transgender women have much lower levels than cisgender men, who have been shown to have a median PSA of 1.0 in previous studies. These values in transgender women are much lower than the commonly used threshold of 4 ng/mL for further prostate cancer evaluation. This suggests that the traditional threshold might be too high for transgender women on estrogen. Moreover, this study highlights the need for assessing the general utility of PSA for prostate cancer screening within this patient population.”
Hoedt emphasized that “current PSA thresholds in prostate cancer screening guidelines may lead to delayed diagnosis of prostate cancer in transgender women on estrogen.”
In the study, 210 patients who underwent 852 PSA tests met the study’s inclusion criteria. The mean age of participants was 60 years old. Median estrogen duration at time of PSA assessment was 4.7 years (range, 0.5-29.9). Most patients (86%) were White, and Black patients were only 2% of the group, the study authors explained.
The authors determined that “PSA distributions were similar in sensitivity analyses using first PSA (median [IQR], 0.08 [0-0.3] ng/mL; 95th percentile, 0.7 ng/mL) and median of all PSAs per patient (median [IQR], 0.06 [0.01-0.2] ng/mL; 95th percentile, 0.5 ng/mL). The highest PSA in the cohort was 2.21 ng/mL.”
They concluded the “usefulness of PSA screening in transgender women receiving gender-affirming hormones remains unknown. For these transgender women who do undergo screening, the optimal cut point to define ‘high risk’ is also unknown.”
Very Low PSA
The study’s findings that “PSA values were very low among transgender women receiving estrogen suggest the historic cut point of 4 ng/mL, which is frequently used as a threshold for further evaluation, is likely far too high a threshold for this population,” study authors recommended.
“In a previous research study of prostate cancer patients, we found that transgender women on estrogen were diagnosed with more advanced disease compared to cisgender men,” Hoedt said. “We suspected this might be due to delayed diagnosis among transgender women. PSA is the primary tool used for prostate cancer screening, and we hypothesized that gender-affirming hormones such as estrogen may lower PSA levels. If this was true, it could mean that these patients don’t meet standard PSA thresholds used for further prostate cancer screening, and that current guidelines may not reflect the needs of this patient population.”
Healthcare professionals who are making decisions about transgender women and prostate cancer “must exercise caution when interpreting PSA values among transgender women on estrogen,” Hoedt suggested.
“Currently, there are no strong, evidence-based guidelines to assess how informative different risk factors are in this population,” Hoedt said. “However, we would recommend continuing to evaluate other known risk factors for prostate cancer such as age, race and family history when evaluating patients. If clinicians perform PSA screenings, they must realize the normal values are much lower and thus the traditional cut-off of 4 ng/mL is likely too high in this population.”
The researchers acknowledged the current study had several limitations, including “lack of a comparison group, potential biases from not knowing PSA testing indications, and inability to access outside records unless documented in VHA records.”
In the future, “further studies are needed to understand the risks and benefits of PSA screening in transgender women receiving estrogen and to establish ideal prostate cancer screening practices. More studies are also needed to examine the experiences of minority transgender women and inequities in prostate cancer screening. In this study’s random sample of transgender women, only 2% of the patients were Black, which aligns with previous studies showing fewer Black transgender women with prostate cancer. However, Black patients make up approximately 16% of the VHA population,” the authors explained.
Another study published in JAMA Network in 2023 described a large case series of transgender women with prostate cancer within the VAHS from January 2000 to November 2022. The researchers explained that “transgender women retain their prostate even after gender-affirmation surgery, so they remain at risk of prostate cancer.”2
The authors found that, “among 449 patients with prostate cancer and transgender identity codes, 155 (35%, an estimated 14 cases per year) were confirmed transgender women with prostate cancer. Of these transgender patients, 116 never used estrogen, 17 formerly used estrogen, and 22 actively used estrogen at diagnosis. All prostate cancer diagnoses were detected by screening.”
The study’s results demonstrate that “prostate cancer occurs in transgender women and isn’t as rare as published reports might suggest. However, rates were lower than expected based on previous prostate cancer incidence estimates in cisgender male veterans. With estimates of 10,000 transgender women in the VA, 33 cases of prostate cancer were expected each year, but this study only observed 14 cases per year. The lower rates may be attributed to less PSA screening because of obstacles such as lack of prostate cancer risk awareness or stigma, the suppressive effects of estrogen on prostate cancer development, or prostate cancers being missed in transgender women due to misinterpretation of ‘normal’ PSA levels among those receiving gender-affirming hormone therapies. In the study, only 8% of transgender women with prostate cancer versus 29% of cisgender male veterans with prostate cancer were Black, which suggests additional disparities based on race and gender identity.”
“We still have a lot to learn about the best ways to diagnose and treat prostate cancer among transgender veterans, and we are excited to be at the forefront of this research to help improve and save lives,” Hoedt said.
- Nik-Ahd F, De Hoedt AM, Butler C, Anger JT, Carroll PR, Cooperberg MR, Freedland SJ. Prostate-Specific Antigen Values in Transgender Women Receiving Estrogen. JAMA. 2024 Jun 26:e249997. doi: 10.1001/jama.2024.9997. Epub ahead of print. PMID: 38922607; PMCID: PMC11209176.
- Nik-Ahd F, De Hoedt A, Butler C, Anger JT, Carroll PR, Cooperberg MR, Freedland SJ. Prostate Cancer in Transgender Women in the Veterans Affairs Health System, 2000-2022. JAMA. 2023 Jun 6;329(21):1877-1879. doi: 10.1001/jama.2023.6028. PMID: 37119522; PMCID: PMC10148974.

