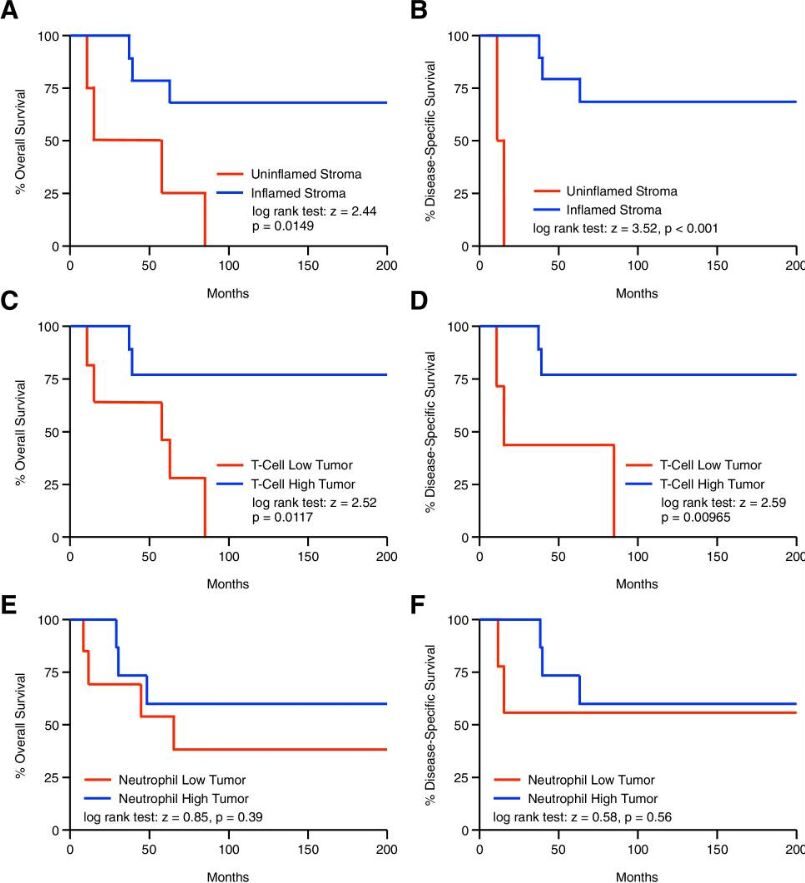
Click to Enlarge: Increased post-treatment tumor-infiltrating lymphocytes are associated with improved overall and disease-specific survival in anal SCC. (A) Kaplan–Meier curve indicating months of overall or disease-specific survival for post-treatment anal SCC patients arranged by (A,B) an inflamed or uninflamed tumor stroma, or the degree of tumor-infiltrating (C,D) T-cells or (E,F) neutrophils
CHICAGO ― The prognosis is favorable for the majority of anal squamous cell carcinoma (SCC) patients; in 70% to 80%, tumors are highly sensitive to standard-of-care chemoradiation.
On the other hand, “outcomes are poor for the 20-30% of patients who are refractory to this approach, and many will require additional invasive procedures with no guarantee of disease resolution,” according to a study in BMC Cancer.1
Researchers from the University of Illinois at Chicago and the Jesse Brown VAMC in Chicago sought to identify patients who are unlikely to respond to the current standard of care chemoradiation protocol. In a single-center retrospective study of 42 patients with anal SCC, the investigators examined a range of objective clinical findings as potential predictors of treatment failure and/or mortality. Participants had previously untreated, non-metastatic anal SCC and related alterations in peripheral as well as tumor-infiltrating leukocyte subtypes to primary therapy success and overall survival.
Results indicated that patients with an increase in total peripheral white blood cells (WBC) and/or neutrophils (ANC) had less favorable clinical outcomes, with increased rates of death and treatment failure.
Using pre-treatment biopsies from 27 patients, the researchers also determined that tumors with an inflamed, neutrophil dominant stroma also had poor therapeutic responses, leading to reduced overall and disease-specific survival.
“Following chemoradiation, we observed uniform reductions in nearly all peripheral blood leukocyte subtypes, and no association between peripheral white blood cells and/or neutrophils and clinical outcomes.,” the authors wrote. “Additionally, post-treatment biopsies were available from 13 patients. In post-treatment specimens, patients with an inflamed tumor stroma now demonstrated improved overall and disease-specific survival, particularly those with robust T-cell infiltration.”
The researchers concluded that, “combined, these results suggest that routinely performed leukocyte subtyping may have utility in risk stratifying patients for treatment failure in anal SCC. Specifically, pre-treatment patients with a high WBC, ANC, and/or a neutrophil-dense tumor stroma may be less likely to achieve complete response using the standard of care chemoradiation regimen, and may benefit from the addition of a subsequent line of therapy.”
Background information in the articles explained that anal squamous cell carcinomas (SCC) are Human papillomavirus infection(HPV)-associated cancers which are most common in immunocompromised patients.
“Though rare,” the authors advised, “the incidence of anal SCC has been steadily increasing in recent years, particularly among select populations including women, persons living with HIV, and transplant patients.”
The advent of the Nigro protocol, a multimodal therapy regimen combining external beam radiation, 5-fluorouracil (5-FU), and mitomycin-C, has greatly improved the prognosis for locally advanced anal SCC, according to the study, which noted that the approach has been the standard of care for decades. The patients for whom the therapy does not work, however, face a 2-year survival rate of 28% and a 5-year survival rate of 0% without additional intervention.
The additional treatment usually includes abdominoperineal resection (APR) is generally indicated as salvage treatment, with inguinal lymph node dissection if indicated, which is a highly invasive procedure, associated with a high rate of wound complications, as well as sexual and urinary dysfunction, or chemotherapy, which has a low success rate. “Hence, there is an urgent need to identify the patients unlikely to achieve satisfactory disease control using the current standard of care in hopes of providing a more effective first-line therapy, thereby limiting the need for invasive or poorly effective treatments and improving long-term survivability,” the authors emphasized.
HPV status clearly predicts clinical outcomes, according to the researchers, but those are ubiquitous in anal SCC, affecting as many as 90% of patients. “Hence, while HPV-positive patients have an improved prognosis, HPV status has limited utility as a prognostic biomarker,” they explained.
The study authors concluded, “Our results suggest that routinely performed leukocyte subtyping may have utility in risk stratifying patients for treatment failure in anal SCC. Specifically, pre-treatment patients with a high WBC, ANC, and/or a neutrophil-dense tumor stroma may be less likely to achieve complete response using the standard of care chemoradiation regimen, and may benefit from the addition of a subsequent line of therapy.”
- Principe DR, Cataneo JL, Timbers KE, Koch RM, Valyi-Nagy K, Mellgren A, Rana A, Gantt G. Leukocyte subtyping predicts for treatment failure and poor survival in anal squamous cell carcinoma. BMC Cancer. 2022 Jun 24;22(1):697. doi: 10.1186/s12885-022-09742-7. PMID: 35751111; PMCID: PMC9229146.

