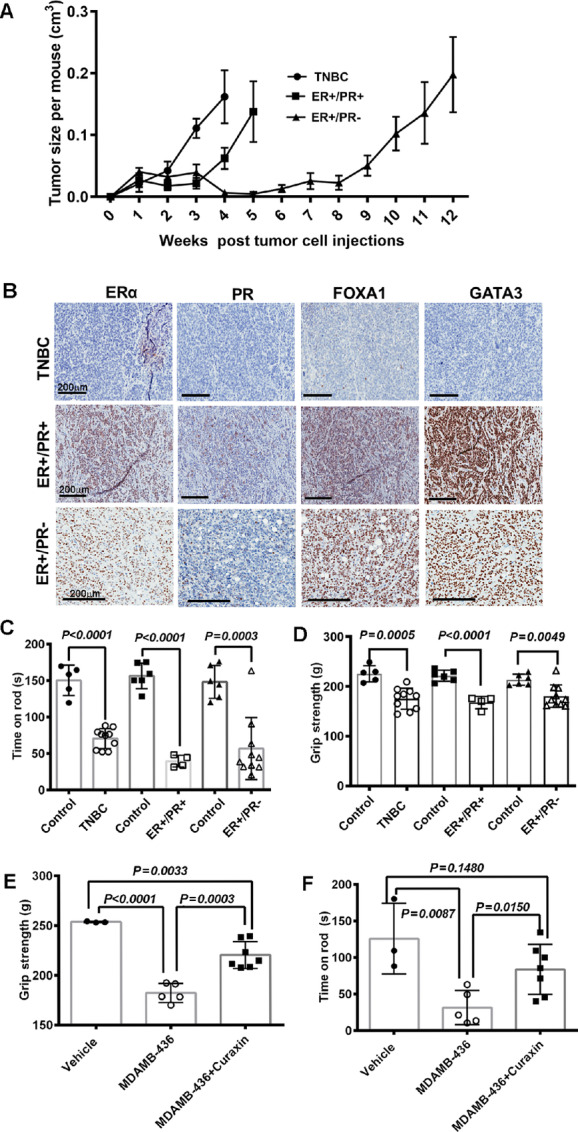
Click to Enlarge: Tumor subtypes differentially affect skeletal muscle function in mice with PDXs. A: Growth rate of PDXs in NSG mice. B: Histology of PDXs confirming their molecular subtype. C: Impaired rotarod performance of mice with PDXs across all tumor subtypes. D: Differential impact of tumors by subtype on grip strength of mice with PDXs. Mice with TNBC tumors had severe loss of grip strength. E: Loss of grip strength was improved by Curaxin (CBL0137) treatment in nude mice with tumors from MDA-MB-436 cells. F: Impaired rotarod performance was ameliorated by Curaxin (CBL0137) in nude mice with tumors from MDA-MB-436 cells. Source: Cancer Research Communications
INDIANAPOLIS — The quality of life for many breast cancer patients is affected by skeletal muscle dysfunction, which is estimated to appear in about 39% of cases.
Researchers from Indiana University and the Richard L Roudebush VAMC, all in Indianapolis, noted that cancer-induced skeletal muscle defects differ in severity between individuals with the same cancer type. “Cancer subtype-specific genomic aberrations are suggested to mediate these differences, but experimental validation studies are very limited,” they explained in Cancer Research Communications.1
In response, the study team used three different breast cancer patient-derived xenograft (PDX) models to correlate cancer subtype with skeletal muscle defects. The PDXs were derived from brain metastasis of triple-negative breast cancer (TNBC), estrogen receptor-positive/progesterone receptor-positive (ER+/PR+) primary breast cancer from a BRCA2-mutation carrier and pleural effusion from an ER+/PR-breast cancer.
“While impaired skeletal muscle function as measured through rotarod performance and reduced levels of circulating and/or skeletal muscle miR-486 were common across all three PDXs, only TNBC-derived PDX activated phospho-p38 in skeletal muscle,” they advised.
With the understanding that mutations in RAS oncogene or its modulators are found in about 37% of metastatic breast cancers, which is often associated with skeletal muscle defects, the researchers sought to further extend their results by generating transformed variants of human primary breast epithelial cells from healthy donors using HRASG12V or PIK3CAH1047R mutant oncogenes.
“Although cells transformed with both oncogenes generated adenocarcinomas in NSG mice, only HRASG12V-derived tumors caused skeletal muscle defects affecting rotarod performance, skeletal muscle contraction force, and miR-486, Pax7, pAKT, and p53 levels in skeletal muscle,” according to the results. “Circulating levels of the chemokine CXCL1 were elevated only in animals with tumors containing HRASG12V mutation. Because RAS pathway aberrations are found in 19% of cancers, evaluating skeletal muscle defects in the context of genomic aberrations in cancers, particularly RAS pathway mutations, may accelerate development of therapeutic modalities to overcome cancer-induced systemic effects.”
Skeletal Muscle Affected
The authors suggested those findings were significant because mutant RAS- and PIK3CA-driven breast cancers can affect the function of skeletal muscle. “Therefore, research and therapeutic targeting of cancer-induced systemic effects need to take aberrant cancer genome into consideration,” they wrote.
Background information in the articles pointed out that age, body composition, disease stage and progression contribute to breast cancer-associated skeletal muscle dysfunction. While knowledge has been limited, it has been assumed aggressive tumor types have greater impact on skeletal muscles of patients.
The current study “observed profound skeletal muscle defects in mice harboring mutant HRAS-driven tumors compared with those with mutant PIK3CA-driven tumors, despite both tumors being adenocarcinomas. These results suggest that breast cancer subtype uniquely impacts skeletal muscle function and, moving forward, it is critical to consider RAS pathway mutations not only in breast cancer therapy but also in breast cancer-induced skeletal muscle defects,” according to the researchers.
They concluded, “Tumor genomic data generated as a part of precision oncology need to be explored in decision-making on treatment options not only for controlling tumor progression but also for reducing systemic effects of cancer.”
The study team cautioned, however, that studies related to mutant RAS oncogene and cachexia in breast cancer “are often met with skepticism by reviewers because of the dogma in the field that both of these are not relevant for breast cancer. Because of this skepticism, significant progress achieved in the RAS field, including the development of mutant RAS-specific inhibitors (56) is not being translated clinically in breast cancer.”
The researchers emphasized, however, that recent advances clarify the role of RAS signaling in metastatic breast cancers and the development of cachexia, which affects about a fourth of breast cancer patients. “We hope results presented in this study would help to overcome this skepticism at least partially and will help to move the field forward,” they added.
- Wang R, Khatpe AS, Kumar B, Mang HE, Batic K, Adebayo AK, Nakshatri H. Mutant RAS-driven Secretome Causes Skeletal Muscle Defects in Breast Cancer. Cancer Res Commun. 2024 May 15;4(5):1282-1295. doi: 10.1158/2767-9764.CRC-24-0045. PMID: 38651826; PMCID: PMC11094532.

