Experts Disagreed on Discontinuation of Long-Term Opioids
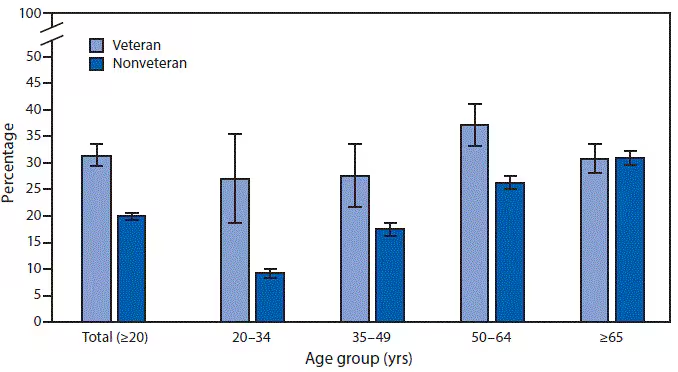
Click to Enlarge: Percentage of Adults Aged ≥20 Years Who Had Chronic Pain, by Veteran Status and Age Group.
* With 95% confidence intervals shown with error bars.
† Based on the response to a survey question that asked “In the past 3 months, how often did you have pain? Would you say never, some days, most days, or every day?” Chronic pain was defined as pain on most days or every day in the past 3 months.
§ Estimates are based on household interviews of a sample of the civilian, noninstitutionalized U.S. population and are derived from the National Health Interview Survey Sample Adult component. Source: National Health Interview Survey, 2019. https://www.cdc.gov/nchs/nhis.htm.
INDIANAPOLIS — A new VA-led study underscored the urgent need for clear guidelines on how best to treat chronic pain, especially when it comes to prescribing opioid pain medications.
“Although long-term opioid therapy (LTOT) for chronic pain has declined, it remains common in the U.S. Providers do not have clinical practice guidelines for vulnerable LTOT patients, in whom both LTOT continuation and tapering to discontinuation pose risks of harm and in whom opioid-use disorder (OUD) is absent,” wrote the authors from the Center for Innovation to Implementation at the VA Palo Alto, CA, Healthcare System and Stanford University School of Medicine in Stanford, CA, and colleagues. Researchers from VAMCs in Ann Arbor, MI; Birmingham, AL; and San Francisco contributed to the research.
In the study, published in Pain Practice, the investigative team used a multiple-case study approach. Five cases were constructed to systematically vary key elements of LTOT continuation and discontinuation harms among patients reporting LTOT’s lack of efficacy (experience of pain and poor function).1
For each, treatment approaches were collected from 28 opioid safety experts identified through their participation in a national policy panel (19 were physicians) and analyzed using template analysis.
Quantitative data indicated that 36% of experts agreed LTOT is beneficial, 36% agreed most LTOT patients should be discontinued, and 57% agreed patients experience harm from tapering and from discontinuation.
“For patients receiving LTOT with harms of continuation and discontinuation, experts recommended attempting a slow taper (even with a prior unsuccessful taper, possibly with adjuvant medications to manage withdrawal) and not maintaining opioid therapy,” the authors advised. “Experts considered switching to buprenorphine, especially if the patient had aberrant behaviors. They also considered adding non-opioid pain therapies (especially re-trying such therapies if they were unhelpful before) and engaging in shared decision-making, although with little consensus on specific approaches.”
Co-Occurring Conditions
They said that some experts emphasized addressing co-occurring conditions related to patient safety, such as alcohol use, mental health symptoms and opioid side effects, adding, that “few experts referenced assessing or addressing OUD or overdose risk.”
“Chronic pain is complex and difficult to treat,” the authors pointed out. “Prescribing opioid pain medications has become controversial but may help some patients.”
Study authors noted the lack of consensus among the experts on how to treat chronic (lasting 3 or more months) noncancer pain. While slightly more than one-third of the experts said that long-term opioid therapy is beneficial, an equal percentage indicated that it should be discontinued, they pointed out.
In fact, more than half of the experts suggested that patients can experience harm from overly rapid tapering and discontinuation, while some recommended attempting a slow taper (even with a prior unsuccessful taper), possibly with addition of medications to manage withdrawal) in order not to maintain opioid therapy.
“The potential harms of opioid pain medication are well known, nevertheless patients can become habituated to them and want their physicians to continue prescribing them. Taking patients off opiates may result in return or worsening of chronic pain, mental health issues, drug seeking and potentially overdose and death. Additionally, these drugs could be used by someone else, possibly winding up on the street,” explained study co-author Kurt Kroenke, MD, of the Regenstrief Institute and the Indiana University School of Medicine. “On the benefit side, these drugs may be helping relieve the patient’s often debilitating pain, which can impact the ability to interact with family, to hold a job, participate in social activities and many other aspects of life.”
Kroenke noted that the substantial number of patients who are prescribed opioid pain medications and continue to experience chronic pain might be good candidates for tapering to a lower dose, prescription discontinuation and moving on to effective, safer treatments for pain.
Based on the expert opinions, “Guidelines on whether to continue or taper opioids prescribed long term may be difficult to utilize given professional liability concerns, changing regulations and health system initiatives, differing provider-patient perspectives on long-term opioid benefits and harms, and some providers’ beliefs that opioid dependence interferes with patients’ objectivity,” the authors wrote. “In the meantime, individual care decisions that involve weighing relative harms should draw on longstanding norms of ethical medical care that call for informed consent and patient-provider conversations grounded in mutual respect.”
The VA reduced the number of veterans with opioid prescriptions by 67% since 2012, from 874,897 veterans in 2012 to 288,820 in 2023.
- Timko C, Lor MC, Kertesz S, Kroenke K, Macia K, Nevedal A, Hoggatt KJ. Management of patients at risk of harms from both continuing and discontinuing their long-term opioid therapy: A qualitative study to inform the gap in clinical practice guidelines. Pain Pract. 2025 Jan;25(1):e13440. doi: 10.1111/papr.13440. Epub 2024 Nov 18. PMID: 39552589.

