SAN FRANCISCO — Chronic heart failure affects an estimated 5% of veterans in the VA Health System, and annual mortality in heart failure patients is 15%. Common preventable risk factors for heart failure include tobacco use, an unhealthy diet, lack of exercise and excessive alcohol intake, according to the national Centers for Disease Control and Prevention.
VA researchers are trying to better understand another—use of the stimulants methamphetamine and cocaine—with the goal of determining who’s at greatest risk before a heart failure diagnosis.
To search for answers, researchers at the San Francisco VAMC turned to the Mind Your Heart Study Cohort, a database of veterans that has been used to look at the impact of PTSD and psychiatric disease on cardiovascular health.
“Because PTSD and psychiatric disease are often comorbidant with stimulant use, the Mind Your Heart database was a particularly useful one to look at the effects of stimulant use on cardiovascular disease,” said Jacqueline DesJardin, MD, a cardiology fellow at the San Francisco VA and lead author of the study presented at the American College of Cardiology’s 72nd Annual Scientific Session in New Orleans. The database contains fairly detailed information about illicit drug use obtained from surveys with each member, as well a variety of other data and tests, including cardiac ultrasounds.1
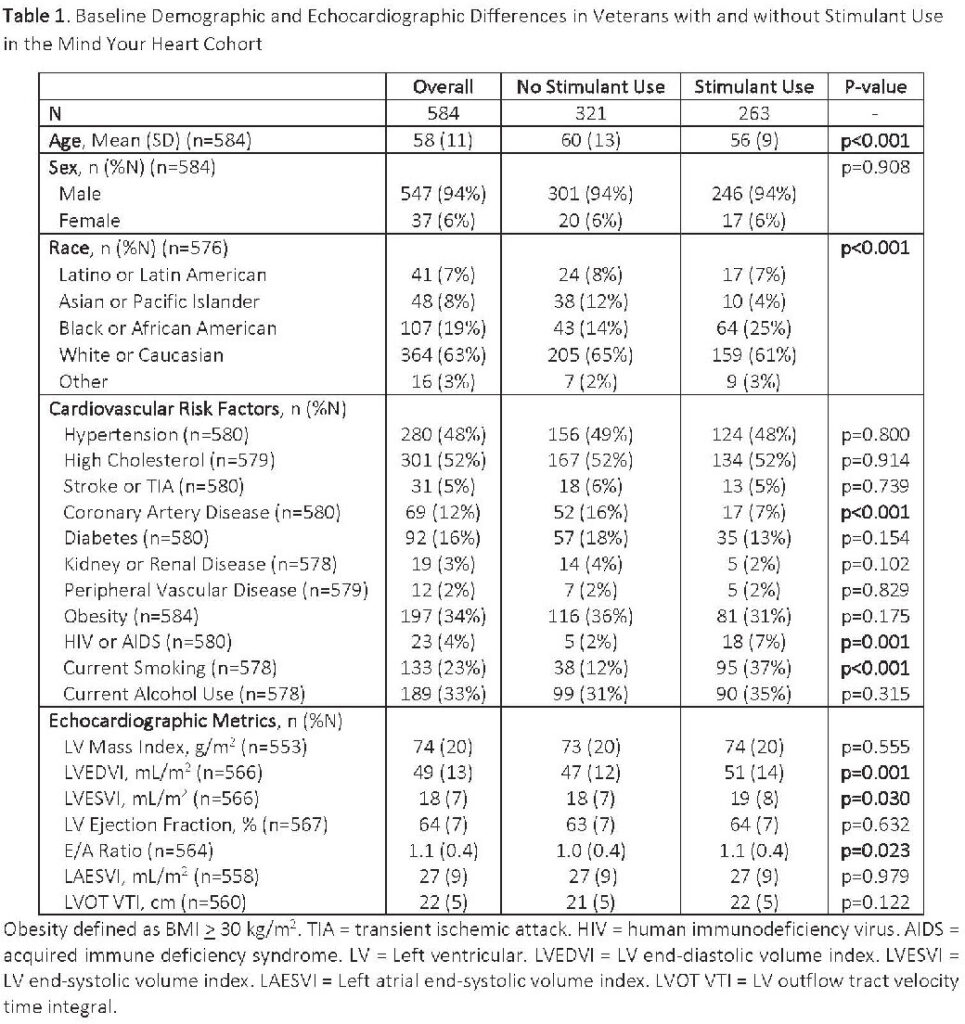
After excluding all veterans with a diagnosis of heart failure, the researchers stratified the remaining 584 veterans in the cohort based on history of stimulant use (45 %) and no stimulant use (55%) and examined cardiac ultrasounds to see if they could detect any changes that were associated with stimulant use, DesJardain said.
Their examination revealed they had larger left ventricular end-diastolic and end-systolic volume indexes (LVEDVI; LVEDSVI) and higher E-to-A ratios. In linear regression models adjusting for age, race, coronary artery disease, HIV status and smoking, stimulant use was associated with higher LVEDVI but not LVESVI or E-to-A ratio. Each additional year of stimulant use was associated with an increased LVEDVI with the greatest increases seen in veterans with current stimulant use, the study showed.
Stimulant-Associated Damage
“So we think that this might be an early sign of stimulant-associated damage to the heart,” said DesJardin, who is now interested in looking forward to the implications of these findings and whether those identified with stimulant use and left ventricle changes go on to develop heart failure. “If that is, in fact, an early sign, we might be able to pick on ultrasound that someone is at particularly high risk of going on to develop methamphetamine [or cocaine]-associated heart failure. A better understanding of who’s at greatest risk could allow more aggressive interventions based on risk”, she said.
A second benefit of the research is that it might allow for the study of drugs to potentially prevent heart failure, DesJardin said. “There are a number of medications that we use to treat heart failure,” she said. “What is unclear is if they prevent heart failure. But it would be interesting, if we could find in people who are at highest risk of developing heart failure; can we treat them with some of these medications to help prevent the onset of heart failure?”
DesJardin said she would also be interested in learning the risks of cocaine versus methamphetamine, which were simply grouped as “stimulants” in the study. “We also have a lot of patients who use multiple substances, so something, teasing it out is not easy. It is going to be hard to differentiate, but I would definitely be interested in that.”
Her ultimate goal, she says, is to make is to make heart failure from a preventable cause—namely stimulant use—preventable. “I’m used to seeing people who are older, in their 70s, getting heart failure. But when I see methamphetamine-associated heart failure, I can see patients in their 20s and their 30s,” she said. “The public health consequences of that are extreme, so I think we really need to do our due diligence to study this population to understand and how to treat not only heart failure but the coexisting substance use disorder and figure out ways to help them. In my opinion, to have a 30-year-old with a preventable cause of heart failure is unacceptable.”
- DesJardain J, Schiller NB, Cohen B, (2023, March 4-6) Left Ventricular End-Disatolic Volume Index Increases with Stimulant Use in a Dose-Dependent Manner [Conference presentation abstract]. Seventy-second Annual Scientific Session of the American College of Cardiology Together with World Congress of Cardiology, New Orleans, LA, United States.