Diagnosis Increased, However, in VHA Patients 65 and Older
Click to Enlarge: Trends in Opioid Use Disorder (OUD) Diagnoses in the Veterans Health Administration From 2005 to 2022 Source: JAMA Network Open
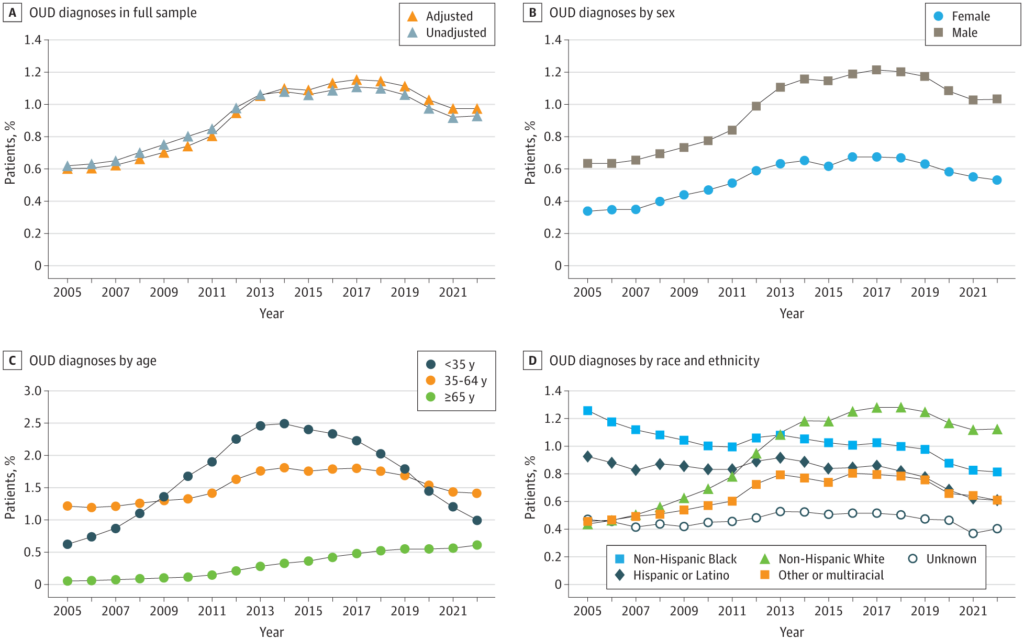
NEW YORK — After peaking at 1.16% in 2017, the prevalence of opioid-use disorder (OUD) among VHA patients declined steadily and was 0.97% in 2022, the most recent date for which data is available.
That’s according to a new Columbia University Irving Medical Center-led cross-sectional study that included approximately 5 million adults per year and determined that the prevalence of OUD increased from 2005 to 2017, reached its apex in 2017 at 1.16% and declined until 2022 to 0.97%.
The study team, which included participation from the VA Puget Sound Health Care System in Seattle and the San Francisco VAMC, advised that the findings “suggest that the prevalence of OUD is declining, although continued public health efforts aimed at recognizing, treating and preventing OUD are warranted,” adding, “Given the personal and social burdens of opioid use disorder (OUD), understanding time trends in OUD prevalence in large patient populations is key to planning prevention and treatment services.”
The study’s final sample size ranged from 4.3 million to nearly 6 million per year, with nearly 90% men.
Results indicated that, overall, the annual percentage of VHA patients diagnosed with OUD almost doubled from 2005 to 2017 (0.60% [95% CI, 0.60%-0.61%] to 1.16% [95% CI, 1.15%-1.17%]; adjusted difference, 0.55 [95% CI, 0.54-0.57] percentage points) and declined thereafter (2022: 0.97% [95% CI, 0.97%-0.98%]; adjusted difference from 2017 to 2022, -0.18 [95% CI, -0.19 to -0.17] percentage points). The trend was found to be similar among:
- Men (0.64% [95% CI, 0.63%-0.64%] in 2005 vs. 1.22% [95% CI, 1.21%-1.23%] in 2017 vs. 1.03% [95% CI, 1.02%-1.04%] in 2022),
- Women (0.34% [95% CI, 0.32%-0.36%] in 2005 vs. 0.68% [95% CI, 0.66%-0.69%] in 2017 vs. 0.53% [95% CI, 0.52%-0.55%] in 2022),
- Those younger than 35 years (0.62% [95% CI, 0.59%-0.66%] in 2005 vs. 2.22% [95% CI, 2.18%-2.26%] in 2017 vs. 1.00% [95% CI, 0.97%-1.03%] in 2022),
- Those aged 35 to 64 years (1.21% [95% CI, 1.19%-1.22%] in 2005 vs. 1.80% [95% CI, 1.78%-1.82%] in 2017 vs. 1.41% [95% CI, 1.39%-1.42%] in 2022), and
- Non-Hispanic white patients (0.44% [95% CI, 0.43%-0.45%] in 2005 vs. 1.28% [95% CI, 1.27%-1.29%] in 2017 vs. 1.13% [95% CI, 1.11%-1.14%] in 2022).
Among VHA patients aged 65 years or older, however, OUD diagnoses increased from 2005 to 2022 (0.06% [95% CI, 0.06%-0.06%] to 0.61% [95% CI, 0.60%-0.62%]). On the other hand, Hispanic or Latino and non-Hispanic Black patients had decreased OUD diagnoses from 2005 (0.93% [95% CI, 0.88%-0.97%] and 1.26% [95% CI, 1.23%-1.28%], respectively) to 2022 (0.61% [95% CI, 0.59%-0.63%] and 0.82% [95% CI, 0.80%-0.83%], respectively).
The authors suggested in JAMA Network Open that substantial public health efforts, including limits on opioid prescribing; implementation of prescription drug monitoring programs; expansion of opioid agonist therapies and greater access to addiction treatment made the difference, among other initiatives.1
“U.S. data show consistent increases in the prevalence of OUD up to 2018,” the researchers pointed out. “However, little is known about more recent trends given that major surveillance surveys were interrupted by the COVID-19 pandemic, precluding the ability to validly merge data from 2020 to 2021 with prior and later years. To our knowledge, no published studies to date included data from 2020 onward, and only two published studies included data as recent as 2019.”
They also decried the lack of recent evidence on OUD trends in the overall population, including trends by key demographic characteristics. “This is an important gap, as OUD and overdose deaths have been shown to disproportionately affect adults who are male, younger than 64 years and non-Hispanic White, although it is unclear how OUD in these subgroups is evolving over time,” according to the authors. “Understanding more recent trends both overall and among demographic groups may therefore aid in 3 goals: (1) assessing the evolution of the current opioid crisis through the lens of OUD, (2) ascertaining whether (and the extent to which) public health efforts have been successful at curbing OUD, and (3) aiding in more effectively targeting scarce resources and messaging to the populations at greatest OUD risk.”
The VHA patient population is not representative of the entire U.S., having higher proportions of men, white individuals, older individuals and those with low income; however, VHA findings on trends and risk factors “have contributed to important improvements in prevention strategies and health care practices nationally and internationally and have generally been consistent with nationally representative data on selected substance use issues,” according to the study.
The authors suggested the positive results “are likely due to the numerous robust efforts within and outside the VHA aimed at combatting the opioid crisis. As early as 2013, the VHA established the Opioid Safety Initiative, including programs to expand nonopioid alternatives for pain and to promote reductions in opioid prescribing. While declines in prescribing were not associated with reductions in fatal overdoses among VHA patients with preexisting OUD, fewer prescriptions were found to be associated with reduced incident cases of OUD among younger, more opioid-naive patients. Among those younger than 35 years, the age category least likely to have long-standing opioid prescriptions, we observed declines in OUD diagnoses starting in 2014.”
The study pointed out that VHA improved access to medications for OUD in primary care. Other initiatives have aimed at using automated flagging of medical records of patients at high risk of opioid overdose, prompting a mandated case review and opening opportunities for intervention and treatment.
“It is noteworthy, however, that declining cases of OUD have occurred in the context of increasing overdose deaths, possibly owing to opioid deaths increasing primarily as a result of an increasingly toxic drug supply, including fentanyl, benzodiazepines, stimulants, and xylazine,” the study advised. “While there were continuous increases in overdose deaths involving synthetic opioids from 2016 to 2020, there were notable declines in overdose deaths from heroin and nonsynthetic prescription opioids during the same period.”
- Gorfinkel LR, Malte CA, Fink DS, Mannes ZL, et. Al. Trends in Opioid Use Disorder in the Veterans Health Administration, 2005-2022. JAMA Netw Open. 2024 Dec 2;7(12):e2451821. doi: 10.1001/jamanetworkopen.2024.51821. PMID: 39705031; PMCID: PMC11662256.

