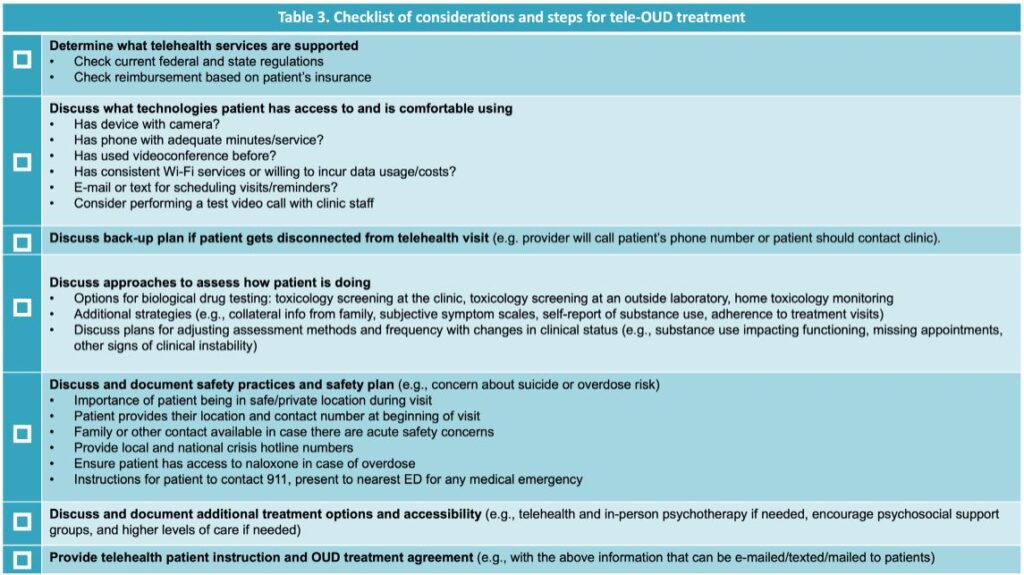
Click to Enlarge: Source: Telehealth for Opioid Use Disorder Toolkit: Guidance to Support High-Quality Care from Providers Clinical Support System and the Substance Abuse and Mental Health Services Administration (SAMHSA).
ANN ARBOR, MI — Implementing new policies during the COVID-19 pandemic reduced barriers to telehealth delivery of buprenorphine treatment for opioid-use disorder for veterans seeking care, a new study reports.
The national retrospective cohort study published in The American Journal of Psychiatry examined the impact of COVID-19 policy changes put into effect in March 2020 on barriers to veterans receiving buprenorphine treatment for opioid-use disorder, including shifts in treatment receipt, treatment retention, delivery modalities (phone, video and in-person visits) and patient demographics.1
The study examined data from veterans with opioid-use disorder receiving care in the Veterans Health Administration (VHA) system from March 2019 through February 2021. Pre-COVID-19 (March 2019 to February 2020) and post-COVID-19 (March 2020 to February 2021) periods were compared. VHA, the largest addiction-treatment provider in the country, provides a view of treatment across the U.S. One of VHA’s key priorities is ensuring access to buprenorphine.
“Our study found that the COVID-19 related policies were associated with helping to sustain increasing trends in buprenorphine care for veterans with opioid-use disorder during the pandemic when we saw other healthcare use decrease,” lead author Lewei (Allison) Lin, MS, assistant professor and director of the Addiction Psychiatry Fellowship Program at the University of Michigan and a research assistant at VA Ann Arbor Healthcare System, told U.S. Medicine.
“We found that care transformed quickly and dramatically after the start of COVID so that the vast majority of visits for buprenorphine occurred via telehealth, with phone visits outnumbering video visits as of February 2021.”
The study found the number of patients receiving buprenorphine increased from 13,415 in March 2019 to 15,339 in February 2021. By February 2021, phone visits were most often used by patients (50.2%, or 4,456 patients), followed by video (32.4%, or 2,870 patients) and in-person (17.4%, or 1,544 patients).
During the pre-COVID-19 period, patients receiving buprenorphine increased by 103 patients per month. After the COVID-19 policy changes, there was a rapid increase of 265 patients in the first month, and this number continued to increase by 47 patients each month. Patients receiving buprenorphine after the COVID-19 policy changes had similar demographic characteristics to those pre-COVID-19, but the percent reaching 90-day retention on buprenorphine decreased from 49.6 percent to 47.7 percent while days on buprenorphine increased from 203.8 to 208.7.
Policy Changes
The key policy changes included eliminating the initial in-person visit requirement for telehealth-delivered buprenorphine treatment under the public health emergency exception to the Ryan Haight Online Pharmacy Consumer Protection Act and expanding coverage of telehealth services to include patients at home by the Center for Medicare and Medicaid Services and other insurance companies. Also, the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Drug Enforcement Administration (DEA) allowed prescribing of buprenorphine treatment through phone visits (rather than requiring video), which was important given disparities in access to internet and digital technologies.
Acceleration of overdose mortality since the start of the COVID-19 pandemic suggests there might be an increase in treatment need or a decrease in treatment utilization in the veteran population, which could be particularly vulnerable to the impacts of COVID-19. This highlights the importance of examining trends in buprenorphine treatment since the start of COVID-19, according to the study. Buprenorphine, an effective medication treatment for opioid-use disorder, is the only effective treatment that can be prescribed in office-based clinics that has been associated with reductions in mortality, Lin explained in an email.
“We found telehealth has played a major role in helping to sustain buprenorphine treatment during the COVID-19 pandemic in a veteran population particularly vulnerable to the effects of pandemic-related health care disruptions,” Lin wrote in an email. “There are active debates right now to determine if these pandemic related policies should be sustained or changed. Our findings suggest that changes to telehealth policies that increase barriers to phone or video telehealth could have implications for patient care and should be carefully considered and disruptions to care should be minimized. We know that risk for overdose increases dramatically when patients stop their buprenorphine; thus, disruptions in care could directly impact patient outcomes.”
This study is one of the first to examine the impact of pandemic-related national telehealth policy changes on care for patients with opioid-use disorder and specifically examined both phone- and video-delivered telehealth effects. Further research is needed to understand the veteran experience, as well as experiences of clinicians, in order to continuously improve the quality of care for veterans with substance-use disorders, Lin wrote.
“Our research suggests that telehealth may have had some benefits in helping sustain access to buprenorphine during the pandemic,” Lin added. “Ideally, in the future, veterans and clinicians can have more options, across the spectrum of telehealth and in-person care, and can make that choice together to optimize care for each veteran.”
- Lin LA, Zhang L, Kim HM, Frost MC. Impact of COVID-19 Telehealth Policy Changes on Buprenorphine Treatment for Opioid Use Disorder. Am J Psychiatry. 2022 Jul 28:appiajp21111141. doi: 10.1176/appi.ajp.21111141. Epub ahead of print. PMID: 35899380.


