The COVID-19 Pandemic Received Blame for Some of the Increase
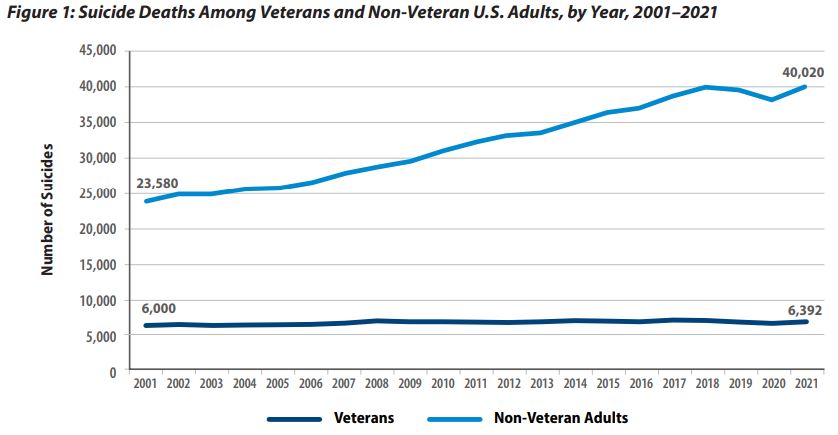
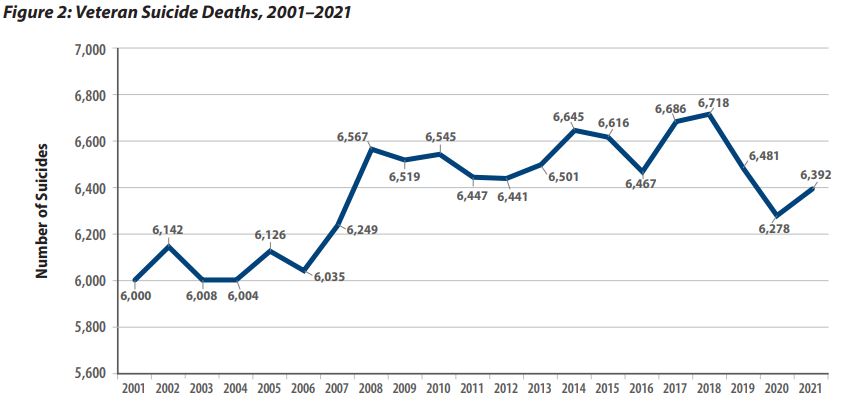
WASHINGTON, DC — A new VA report revealed that 6,392 veterans died by suicide in 2021, the most-recent year for which data was available. That was 114 more than in 2020.
The National Veteran Suicide Prevention Annual Report is the largest national analysis of veteran suicide. The VA pointed out that 2021 was the first full year of the COVID-19 pandemic and suggested that might have led to greater financial strain, housing instability, anxiety and depression levels, as well as barriers to healthcare.
In a press release, the VA further noted that all of those factors “are known to be associated with increased risk of suicide for veterans and non-veterans alike.” The report authors advised that the number of non-veteran suicides also increased to 40,020 deaths in 2021, which is 2,000 more than in 2020.
Another possible issue, according to the report, was the increase in firearm availability in 2021, which it said is proven to increase both the risk of suicide and the risk of dying during a suicide attempt.
“There is nothing more important to VA than preventing veteran suicide—nothing,” said Secretary of Veterans Affairs Denis McDonough. “One veteran suicide will always be too many, and we at VA will use every tool to our disposal to prevent these tragedies and save veterans’ lives.”
The VA said ending veteran suicide is its top clinical priority and a central part of President Joe Biden’s Unity Agenda.
According to the new data, in 2021, suicide was the 13th-leading cause of death for veterans overall and the second-leading cause of death among veterans younger than 45. Of the deaths, 6,042 occurred in male veterans and 350 in female veterans.
The unadjusted rate of suicide in 2021 among U.S. veterans was calculated at 33.9 per 100,000, up from 32.6 per 100,000 in 2020. “In 2021, unadjusted suicide rates were highest among veterans between ages 18- and 34-years-old, followed by those aged 35- to 54-years-old,” according to the new report.
As for race and ethnicity, in 2021, the unadjusted suicide rate was 46.3 per 100,000 for American Indian or Alaska Native veterans; 36.3 per 100,000 for white veterans; 31.6 per 100,000 for Asian, Native Hawaiian or Pacific Islander veterans; 17.4 per 100,000 for Black or African-American veterans; and 6.7 per 100,000 for veterans of multiple races. In 2021, the unadjusted suicide rate was 19.7 per 100,000 for veterans with Hispanic ethnicity, and it was 33.4 per 100,000 for other veterans.
Since 2021, VA has implemented several interventions to better support veterans in crisis, including:
- offering no-cost health care to veterans in suicidal crisis at VA or non-VA facilities;
- launching the 988 (then press 1) to help veterans connect more quickly with the Veterans Crisis Line;
- partnering with community-based suicide prevention organizations to provide veterans with on-the-ground support;
- expanding firearm suicide prevention efforts; and
- encouraging veterans to reach out for help through a national veteran suicide prevention awareness campaign.
More than 33,000 veterans have opted for free emergency healthcare, while use of the Veterans Crisis Line has increased 12.1%, and VA’s support website has received more than 3.5 million visits, according to the VA.
“We will do everything in our power to learn from this report and use its findings to help us save lives,” said VA Under Secretary for Health Shereef Elnahal, MD. “It will take all of us—working together—to end veteran suicide, and we will not rest until that goal becomes a reality.”
Before 2021, veteran suicide had decreased two years in a row—from 6,718 veteran suicides in 2018 to 6,278 in 2020. This report is based on verified data from the national Centers for Disease Control and Prevention, as well as the DoD.
Key Areas of Hope
“When looking at increases in rates from 2020 to 2021, the age- and sex-adjusted suicide rate among veterans increased by 11.6%, while the age- and sex-adjusted suicide rate among non-veteran U.S. adults increased by 4.5%,” the report noted, adding, “Hope is essential to life and hope serves an important role within suicide prevention efforts. Within the challenges faced in 2021, key areas of hope emerged.”
From 2020 to 201, those included:
- Suicide rates fell by 8.1% for veteran men aged 75-years-old and older.
- Among recent VHA users between ages 55- and 74-years-old, the suicide rate fell by 2.2% overall (-0.6% for men, -24.9% for women). (Recent user is defined as veterans who received VA medical care in the past two years.)
- Among male recent VHA users, suicide rates fell by 1.9% for those aged 18- to 34-years-old.
- Among male recent users, suicide rates fell by 8.6% for those aged 75-years-old and older.
- Among male veterans not in VHA care who were aged 75-years-old and older, the suicide rate fell by 7.8%.
- Other significant findings from 2001 to 2021include that:
- The suicide rate among recent VHA users with mental health or substance-use disorder diagnoses fell from 77.8 per 100,000 to 58.2 per 100,000 in 2021.
- Suicide rates fell for recent users with diagnoses of sedative-use disorder (-40.4%), depression (-32.9%), posttraumatic stress disorder (-27.6%) and anxiety (-26.9%).
- Recent VHA users’ suicide rates grew more slowly across 20 years when compared to rates of veterans without Recent VHA use.
“From 2001 to 2021, age-adjusted suicide rates rose 24.5% for male veterans with recent VHA use and 62.6% for male veterans without recent VHA use,” the authors wrote. “Age-adjusted suicide rates rose 87.1% for female veterans with recent VHA use and 93.7% for female veterans without recent VHA use.”
The report also advised that, from 2011-2012 to 2020-2021, the suicide rate among veterans in VHA care with diagnoses related to gender identity fell from 267.9 per 100,000 person-years to 84.6 per 100,000 person-years.
“This report reflects the complexity of suicide inherent in the veteran population, and the United States as a whole, in the context of 2021,” the authors explained. “Suicide prevention entails numerous and complex risks and protective factors across individual, relational, community and societal levels. Within 2021, veterans and the entire U.S. population directly faced health and mortality effects of the COVID-19 pandemic. Weekly U.S. COVID-19 deaths peaked, ebbed, and climbed anew across 2021. By year’s end, over 837,000 Americans had died from COVID-19 since the pandemic began, including over 469,000 Americans who perished from COVID-19 in 2021 alone.”
The report further noted that, in 2020 and 2021, COVID-19 was the third-leading cause of death in the United States, both overall and for veterans. More than 52,500 veterans died from COVID-19 IN 2020 and 60,356 in 2021.
“Veteran deaths from COVID-19 in 2020, and 60,356 in 2021,” the study authors pointed out. “Veteran age- and sex-adjusted all-cause mortality rates were 13.7% higher in 2020-2021 than in 2017-2019.”
Because of the pandemic, according to the report, the U.S. faced greater financial strain, housing instability, anxiety and depression levels, barriers to healthcare and increased firearms availability, the authors wrote, adding that all of those are associated with heightened suicide risk.
“With the increased purchasing of firearms noted in 2020 and 2021, those who purchased and owned firearms were more likely than non-firearm owners to report experiencing thoughts of suicide, and first-time firearm purchasers were more likely to report suicidal ideation,” the authors explained. “In 2021, potential further distress was experienced by many as a result of social conflict and political violence. Veteran distress increased from fall 2019 to fall and winter 2020, with evidence of the highest increases in distress among veterans aged 18- to 44-years-old and among women veterans. These increases in reported distress were associated with increasing socioeconomic concerns, greater problematic alcohol use and decreased community integration.”
In fact, the review pointed out that veterans were found to experience more mental health concerns than non-veterans from the pandemic.
“We need to creatively address the needs of those at risk who may never seek mental health services and who may have other risk factors outside of mental health (e.g., pain, cancer, sleep disturbance) through expansion of suicide screening, assessment, and safety planning into all medical settings, within VHA and within community care,” the report stated.