The mortality burden associated with bacterial bloodstream infections is substantial in the MHS, with about 1 in 4 patients dying within 1 year of a bacterial bloodstream infection diagnosis, according to a recent study.
Small Set of Risk Factors Identified for Subsequent Veteran Suicide
The standardized suicide risk assessment that has been implemented across the VHA healthcare system appears to only identify a few concepts that are associated with subsequent suicide, including suicidal ideation, firearm access and preparatory behaviors, according to a recent study.
Fluoroquinolones Don’t Raise Risk of Aortic Aneurysm, Dissection After All
Fluoroquinolones (FQs) have long been a standard treatment for urinary tract infections (UTIs), offering effective relief for millions of patients worldwide.
VA Plans to Phase Out Gender-Affirming Care for Transgender Veterans
VA has announced that it will be phasing out gender-affirming care for veterans. This is being done, officials said, in response to President Donald Trump’s Executive Order 14168, which excludes transgender people from the government’s definition of gender.
HBV Patients With Diabetes at High Risk of HCC, Other Outcomes
Chronic hepatitis B patients who have two or more metabolic diseases have a significantly higher risk of cirrhosis, overall death and non-liver-related death
Deployed Vietnam Veterans Might Not Have Higher Risk of Bile Duct Cancer
For a half-century, Vietnam veterans have been assumed to have a greater risk of dying of cholangiocarcinoma (CCA), a form of bile duct cancer. A new study suggested that might not be the case, however.
Mailed Outreach for HCC Screening Is Cost-Effective
Mailed outreach significantly increased screening vs. visit-based screening in patients with cirrhosis who are at high risk for hepatocellular carcinoma (HCC).
Congressional VA Committee Members Seek to Mitigate Staff Cuts
The Trump administration’s plan to cut approximately 80,000 employees from VA is receiving pushback from both Republicans and Democrats in Congress.
Military Surgeons Raise Alarm About Combat-Casualty Readiness
The current state of combat-casualty readiness in the military health system has degraded to the point where the country is unprepared to care for the casualties that would result from a major conflict, experts told Congress last month.
Automated Insulin Delivery Safe, Effective for Type 2 Diabetes
Automated insulin delivery (AID) outperformed continuous glucose monitoring alone in Type 2 diabetes patients treated with insulin, according to a new study.
Dietary Cholesterol Intake Directly Linked to Heart Attack Risk in Veterans
Veterans with a higher dietary intake of cholesterol are at increased risk of having a heart attack, according to a recent study that shows a direct link between dietary cholesterol intake and heart attack risk.
Sudden Cardiac Arrest Survival High in Military, but More Prevention Called For
Sudden cardiac arrest is a silent and often fatal event that strikes without warning, even among those in peak physical condition. In the civilian world, survival rates for out-of-hospital cardiac arrest are alarmingly low.
Prolonged Exposure Plus Topiramate Improved PTSD Symptoms, AUD
A combination of prolonged exposure (PE) and topiramate, a medication developed to treat seizures, was more effective than PE and placebo in lessening posttraumatic stress disorder (PTSD) symptoms, according to a new study.
Women Veterans With Substance Abuse More Likely to Die by Suicide
Among U.S. military veterans with addiction diagnoses, women are more likely to die by suicide than men and at younger ages, according to a new study.
Greater TBI Severity Linked to Higher Risk of Alcohol-Use Disorder
U.S. military veterans with traumatic brain injuries were more likely to develop alcohol-use disorder (AUD) and experience increased mortality, even after adjusting for demographic and clinical factors.
There Is Nothing So Useless as Doing Efficiently That Which Should Not Be Done at All
The ongoing assault on America’s health infrastructure has been brutal to watch. The selection of Robert F. Kennedy Jr. as the 26th secretary of the U.S. Department of Health and Human Services (HHS) marks a low point in the department’s leadership history. That decision is already potentially contributing to increased morbidity and mortality within U.S. borders with the recent resurgence in measles cases.
Peer Support Program Benefited Well-Being of Women Veterans, Decreased PTSD, Depression
Women veterans who participated in a peer-led, social support group showed improvements in well-being outcomes, including a greater sense of belonging, higher quality of life and decreased post-traumatic stress disorder (PTSD) and depression, according to a recent study.
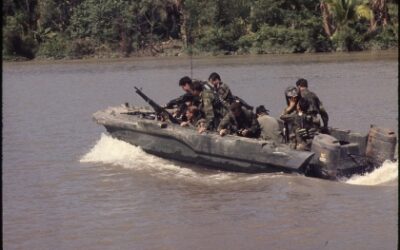
More Than 50 Years Later, Vietnam War Still Affects Veteran Health
More than a half-century after the United States escalated involvement in the Vietnam War by sending significant combat troops, veterans still face significant psychological and physical health challenges related to their employment.
Non-VA Services Reveal Hidden Biases in VA Hospital Performance Metrics
As the veteran population ages and healthcare options expand, it might be beneficial for the VHA to reassess how it evaluates hospital performance, a new study suggested.
2023-to-2024 XBB.1.5 COVID-19 Vaccines Weren’t Effective Over Long Term
Serious concerns were raised in a new VA study about the effectiveness of COVID-19 vaccines targeting the XBB.1.5 Omicron variant, which were introduced in September 2023.
Aligning Total Joint Arthroplasty Outcomes With Patient Expectations
Patient-reported outcome measures are increasingly integrated into quality assessments following total joint arthroplasty (TJA), but patient perceptions of quality paired with the phase of surgical care has not been described, according to a new report.
High Plantar Fasciopathy Rates in U.S. Military
U. S. armed forces have high rates of ankle and foot injuries and mean medical and personnel costs for the DoD.
Veterans’ White-Matter Volume Affected by Physical Activity Level
Trauma exposure affects cardiovascular, cerebral and mental health, causing declines.
PTSD in Veterans With HIV Leads to More Antiretroviral Therapy Nonadherence
In veterans with HIV, having post-traumatic stress disorder (PTSD) increased the likelihood of being nonadherent with their HIV treatment and requiring modification to their HIV treatment, according to a recent study.
Updated VA/DOD Stroke Rehabilitation Guidelines Enhance Patient Care
Revised treatment algorithms, 24 new recommendations and an expanded literature review on complementary and integrative health (CIH) approaches
VA Committee Hears About Challenges Getting Community Mental Healthcare
The Republican focus on further expanding VA-funded community care has been fueled, in part, by reports from veterans and service organizations detailing the hurdles they have had to go through to obtain care for themselves or their clients.
CVD, CKD Combine to Increase Surgical Mortality
What are the interactive effects of cardiovascular disease (CVD) and chronic kidney disease (CKD) on long-term mortality following major operations?
How Different Heart Failure Types Are Affected by CKD
Chronic kidney disease (CKD) is defined by the KDIGO (Kidney Disease: Improving Global Outcomes) guideline as abnormal kidney structure or function, present for more than 3 months, with implications for health.
Decreasing Renal Function Affects PAD Treatment
What is the impact of the severity of chronic kidney disease (CKD) on mortality and major adverse limb events (MALE) after endovascular revascularization of the superficial femoral artery (SFA)?
Happiness Levels in U.S. Military Veterans Similar to General Population
Overall, U.S. military veterans report happiness levels that are only slightly lower than the general population, despite potentially traumatic experiences during deployment.