CHARLESTON, SC—More than half of the patients treated by VA are also Medicare eligible, and that is increasing the risk for a range of prescription medication problems—from chronic disease medication nonadherence to opioid overdoses—among dual users.
The issue has become so serious that VA and the Centers for Medicare & Medicaid Services recently announced an agreement to improve drug safety monitoring of prescriptions. The agreement, formalized in March, will give VA the ability to monitor medical prescriptions issued outside the VA through Medicare Part D.
That likely will be welcomed by pharmacists and other healthcare providers at the VA. A study in the Annals of Pharmacotherapy recently pointed out that, while dual health system use might provide increased access to physicians, medications and other health care resources, it also can increase the complexity and coordination of medication regimens.1
The difficulty related to receipt of prescriptions outside the VA also raises questions about unintended consequences when the new VA MISSION Act, which loosens restrictions on VA patients getting outside care, is fully implemented.
In one study, a team led by researchers from the Ralph H. Johnson VAMC and the Medical University of South Carolina, both in Charleston, sought to evaluate the effect on medication adherence for veterans with dual health care system use—VA and Medicare—when obtaining prescription antihyperglycemic medications to treat diabetes.
The longitudinal cohort study used VA and Medicare data from 2006 to 2010. The study team estimated medication adherence by calculating annualized drug class-level proportion of days covered; PDC greater than 80% was considered adherent.
The research involved more than 250,000 veterans with diabetes, with 27.9% of them defined as pharmacy system dual users. The study noted that mean age was 77.5 years, and nearly all had multiple comorbidities (mean count 10.2).
Nonadherence to Diabetes Drugs
Results indicated that, during follow-up, 75% of VA-only users were deemed adherent to diabetes prescriptions, compared with 63% of dual users. In adjusted models, dual prescription benefit use from VA/Medicare was associated with 39% lower odds of medication adherence (odds ratio [OR] = 0.61; 95% CI = 0.60-0.61).
Furthermore, the researchers emphasized, medication adherence significantly worsened with each additional diabetes medication (OR = 0.65; 95% CI = 0.64-0.65) and significantly decreased over time (OR = 0.95 per year; 95% CI = 0.95-0.96).
“These data suggest that veterans utilizing VA and Medicare to obtain diabetes prescriptions are significantly less likely to be adherent,” study authors concluded.
Medication Supply
Similar problems were identified last year in a study led by researchers from the Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System, Pittsburgh. The study in Health Services Research evaluated the effect of dual use of VA/Medicare Part D drug benefits on antihypertensive medication supply in older veterans with dementia.2
The national review linked 2007-2010 VA and Medicare utilization and prescription records for 50,763 dementia patients with hypertension.
Patients were classified as VA-only, Part D-only or dual VA/Part D users of antihypertensives. Their antihypertensive medication supply in 2010 was classified into one of four categories:
- Appropriate supply of all prescribed antihypertensive classes,
- Undersupply of more than one class with no oversupply of another class,
- Oversupply of more than one class with no undersupply, or
- Both undersupply and oversupply.
Researchers determined that dual prescription users were more likely than VA-only users to have undersupply only (aOR = 1.28; 95 percent CI = 1.18-1.39), oversupply only (aOR = 2.38; 95 percent CI = 2.15-2.64), and concurrent under- and oversupply (aOR = 2.89; 95 percent CI = 2.53-3.29), versus appropriate supply of all classes.
The study reported that 78% of VA outpatient users obtained all their medications from VA only, 20% obtained medications from both VA and Medicare Part D (dual-users), and 2% obtained all medications from Medicare Part D only.
“Obtaining antihypertensives through both VA and Part D was associated with increased antihypertensive under- and oversupply,” study authors wrote. “Efforts to understand how best to coordinate dual-system prescription use are critically needed.”
VA estimated that more than 570,000 veterans have dementia and, of those, approximately 40% seek care in VA medical facilities. “Care coordination for persons with dementia is challenging for healthcare systems under the best of circumstances,” the agency said on its Health Services Research and Development Service website. “The average dementia patient has four comorbid illnesses, receives care from five different providers and uses an average of six different prescription medications. These coordination challenges are exacerbated in Medicare-eligible Veterans who receive care through both Medicare and VA.”
“While dual eligibility for healthcare coverage may offer veterans greater flexibility for accessing medical care, seeking prescriptions across uncoordinated systems may increase the risk of unsafe medication prescribing—particularly in veterans who may have difficulty relaying complex information across VA and non-VA providers,” the VA noted.
Misuse of Opioids
One of the primary drivers of the drug safety monitoring agreement between the VA and CMS was misuse of opioids. Some of that concern was fueled by a study published recently in Annals of Internal Medicine. It found that, among veterans enrolled in VA and Part D, dual use of opioid prescriptions was independently associated with death from prescription opioid overdose.3
“This risk factor for fatal overdose among veterans underscores the importance of care coordination across health care systems to improve opioid prescribing safety,” wrote authors from the VA Pittsburgh Healthcare System, the University of Pittsburgh and Brown University.
“VA is committed to patient safety, and our robust medication surveillance systems are part of that commitment,” said VA Secretary Robert Wilkie in announcing the collaboration. “This agreement greatly enhances medication safety for veterans by providing better oversight of drugs that veterans may be able to obtain from both agencies.”
By incorporating prescriptions dispensed through Medicare, VA providers have access to more accurate information about the medications used by its patients, the agency said, adding that information sharing should help avoid adverse drug interactions, duplication of use and greater risk of adverse drug events, including overdoses.
“This agreement represents a new level of information sharing between VA and CMS, which will improve care coordination and better protect our beneficiaries,” said CMS principal deputy administrator for Operations and Policy Kimberly Brandt. “Leveraging data is a key element of CMS’ efforts to combat the opioid epidemic, and we look forward to continued collaboration with VA on this important issue.”
The opioid use study noted that more than half of VA beneficiaries are also covered by Medicare and can choose to receive their prescriptions from VA or from Medicare-participating providers, cautioning, “Such dual-system care may lead to unsafe opioid use if providers in these 2 systems do not coordinate care or if prescription use is not tracked between systems.”
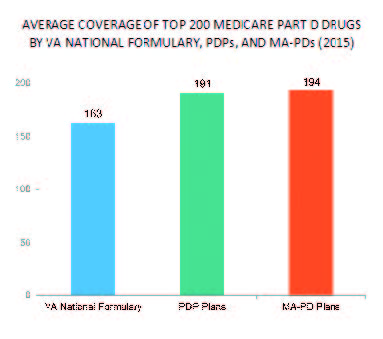
Yet, differences in coverage between the VA and healthcare system make using both advantageous. A 2015 analysis from healthcare consultant Avalere found that the VA national formulary covered 163 of the top 200 most-prescribed Medicare Part D drugs, compared to 191 for Medicare prescription drug plans and 194 for Medicare Advantage prescription drugs plans.
The study matched 215 veterans who died of a prescription opioid overdose in 2012 or 2013 to 833 living control patients on the basis of date of death, using age, sex, race/ethnicity, disability, enrollment in Medicaid or low-income subsidies, managed care enrollment, region and rurality of residence and a medication-based measure of comorbid conditions. Participants, who had a mean age of 57.3, were 90% male and 84% non-Hispanic white.
Researchers determined that 60 case patients (28%) and 117 control patients (14%) received dual opioid prescriptions. Results indicated that dual users had significantly higher odds of death from prescription opioid overdose than those who received opioids from VA only (odds ratio [OR], 3.53 [95% CI, 2.17 to 5.75]; P <0.001) or Part D only (OR, 1.83 [CI, 1.20 to 2.77]; P = 0.005).
1. Taber DJ, Ward R, Axon RN, Walker RJ, Egede LE, Gebregziabher M. The Impact of Dual Health Care System Use for Obtaining Prescription Medications on Nonadherence in Veterans With Type 2 Diabetes. Ann Pharmacother. 2019 Feb 6:1060028019828681. doi: 10.1177/1060028019828681. [Epub ahead of print] PubMed PMID: 30724092.
2. Thorpe CT, Gellad WF, Mor MK, Cashy JP, Pleis JR, Van Houtven CH, Schleiden LJ, Hanlon JT, Niznik JD, Carico RL Jr, Good CB, Thorpe JM. Effect of Dual Use of Veterans Affairs and Medicare Part D Drug Benefits on Antihypertensive Medication Supply in a National Cohort of Veterans with Dementia. Health Serv Res. 2018 Dec;53 Suppl 3:5375-5401. doi: 10.1111/1475-6773.13055. Epub 2018 Oct 16. PubMed PMID: 30328097; PubMed Central PMCID: PMC6235809.
3. Moyo P, Zhao X, Thorpe CT, Thorpe JM, Sileanu FE, Cashy JP, et al. Dual Receipt of Prescription Opioids From the Department of Veterans Affairs and Medicare Part D and Prescription Opioid Overdose Death Among Veterans: A Nested Case–Control Study. Ann Intern Med. 2019;170:433–442. doi: 10.7326/M18-2574.

