
Kim Joiner, the acting principal deputy assistant to the secretary of defense for public affairs, pins a Vietnam veteran lapel pin on a veteran during an observance of Vietnam War Veterans Day at the Vietnam War Memorial in Washington last year. Many veterans of that war are now in need of long term care. DoD photo by Army Sgt. Amber I. Smith,
WASHINGTON—Legislators are referring to it as the “silver tsunami”—the wave of Vietnam-era veterans who are entering their later years and who will increasingly require long-term care from VA over the next decade. Both lawmakers and veterans’ advocates are concerned that this increase in older veterans seeking care will compound the department’s already-existing shortage of care providers.
Of the 19 million veterans in the United States today, 9 million are 65 years or older. This is the largest age cohort of veterans and is expected to remain so for decades. Of these older veterans, about 3.2 million are enrolled in VA healthcare, with half of those having service-connected disabilities that entitle them to VA’s institutional care services.
“One of the largest generations in American history is entering their later years,” declared Rep. Julia Brownley (D-CA), VA Health Subcommittee Chair at a hearing last month. “Compounding this demand is an issue this subcommittee knows well—a harrowing shortage of providers. The Institute of Medicine predicts that, by 2023, the U.S. will need 3.5 million doctors and nurses to care for seniors.”
“In recent years, VA has focused on community care and caregiver programs,” she added. “While these are essential for VA to get right, the scale of the silver tsunami is something that VA cannot afford to get wrong.”
VA’s long-term care programs currently serve more than 500,000 veterans. All veterans enrolled in VA are eligible for some kind of long-term care services, and VA must cover the full cost of nursing care for veterans with a service-connected disability rated 70% or higher and need long-term care because of that disability.
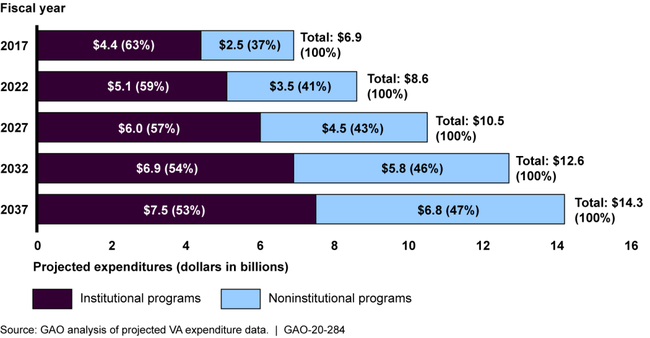
According to a Government Accountability Office report released last month, demand for long-term care at VA increased 14% between 2014 and 2018, while spending increased 33%. VA projects that demand will continue to increase and spending will double by 2037.
The report noted three key challenges VA will face in order to meet that demand: workforce shortages, geographic alignment of care and meeting veterans’ needs for specialty care.
Testifying before the subcommittee, Theresa Boyd, DO, assistant deputy under secretary for health for clinical operations, noted that VA has recognized caring for older veterans as a priority for decades.
“The aging of the veteran population has been more rapid and represents a greater proportion of the patient population than other healthcare systems,” Boyd said. “Addressing the needs of aging veterans was recognized as a priority in 1975, which led to the creation of the GRECCS, or Geriatric Research Education and Clinical Centers), which serve as an incubator for health and health systems relative to older veterans.”
Better Goals Needed
However, the GAO report stated that while VA has acknowledged the challenges it faces and developed some plans to meet them, the department has yet to establish measurable goals, such as specific staffing targets or specific targets for providing telehealth to veterans in rural areas.
Creating these metrics can be difficult, as VA currently operates 14 long-term care programs and lacks a consistent approach to managing them. At some VAMCs where there are no Geriatrics and Extended Care staff, long-term care programs might be operated by one or more departments within the hospital, such as the nursing or social work departments.
“GEC officials told us this fragmentation hinders standardization and the ability to get veterans the appropriate care,” the GAO report states.
Officials also told GAO investigators that VAMCs use different approaches to assess the amount of noninstitutional long-term care veterans need. While GEC has developed a tool to improve consistency of those recommendations, VA has not required the tool to be used at all of its facilities.
Demand for noninstitutional care, such as telehealth, home-based primary care, home hospice and community residential care are the areas VA expects to grow the most over the next decade.
“VA predicts demand for care will continue to shift from institutional settings such as nursing homes to more noninstitutional settings such as aid in the home with home health aids,” explained Nikki Clowers, GAO’s managing director for health care. “Spending on noninstitutional programs is expected to increase by 137% by 2037 while spending on institutional programs will increase by about 70% during this time frame.”
Boyd told legislators that VA has agreed with GAO’s recommendations regarding standardization of long-term care programs and creating measurable goals.
“We take GAO’s observations seriously,” she said. “We have a mismatch. Our brick and mortar was [built] many, many, many years ago, and our veteran populations have moved.”
Boyd also said that noninstitutional programs are not only less expensive but are what most veterans want in their long-term care.
“Veterans want to spend as much of their time as possible at home,” she explained. “That means shifting resources to in-home programs. That will save us money on one side, but it’s also the right thing to do for veterans and for their health.”

