IOWA CITY, IOWA — High rates of diabetes, obesity, smoking, and other risk factors elevate veterans’ risk of peripheral artery disease (PAD) and critical limb ischemia. That puts them at greater risk of limb amputations and mortality.
More than 40% of veterans are obese and approximately one-third have a diagnosis of hypertension. Almost 25% of veterans have diabetes; about the same percentage smoke.
Those factors put them at risk for atherosclerosis, the primary cause of peripheral artery disease. Critical limb ischemia is an advanced stage of PAD in which severe blockage of the arteries inhibits blood flow to the hands, legs, and feet. CLI causes pain, slows healing of wounds, and can lead to gangrene and amputation. It also raises mortality risk, with half of patients dying within five years of diagnosis.
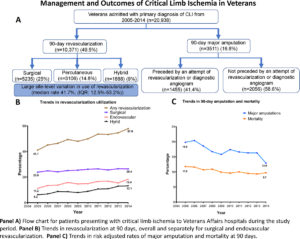
Between 2005 and 2014, 20,938 veterans were discharged from a VA facility with a diagnosis of critical limb ischemia, according to a recent study conducted by researchers with the VA’s Comprehensive Access and Delivery Research and Evaluation group at the Iowa City VAMC and colleagues at the University of Iowa Carver College of Medicine in Iowa City, IA. The study was published in Circulation: Cardiovascular Interventions.1
The team conducted a retrospective analysis of patient records to determine the rate at which veterans received guideline-concordant therapies and how treatment affected rates of amputation and mortality.
“The American College of Cardiology and American Heart Association guidelines recommend that patients with critical limb ischemia get any form of revascularization, to avoid amputations and to improve quality of life, as long as the anatomy is feasible,” co-author Amgad Mentias, MD, a cardiologist, at the University of Iowa Carver College of Medicine, told U.S. Medicine.
Over the decade studied, the rate of revascularization with 90 days of hospitalization for CLI rose significantly. Overall, the revascularization rates increased from 41.2% to 57.9%, with endovascular procedures rising from 11.2% to 18.4% and surgical procedures nudging upward from 23.8% to 26.4%. Hybrid procedures more than doubled during the period, increasing from 6.2% to 13.1%.
As expected based on the strong recommendations for revascularization from leading societies, outcomes for those who had either surgical bypass or the less-invasive endovascular procedure to restore blood flow to the extremities were better than for those who did not.
Lower Mortality
“In our study, there was an association between any form of revascularization and lower mortality and amputation in our adjusted model,” Mentias said.
Ninety-day risk-adjusted mortality declined from 11.8% in 2005 to 9.7% in 2014. Over the same period, major amputations decreased from 19.8% to 12.9% in the three months following discharge.
“Over the past decade, use of revascularization increased among veterans with CLI, which was accompanied by a reduction in mortality and major amputation,” the authors found.
Patients who had a procedure to restore blood flow had a 55% reduction in mortality risk and 77% reduction in risk of amputation within 90 days compared to those who did not have a revascularization procedure.
Despite the marked improvement over the decade, “opportunities to further improve care in this high-risk population still remain,” the authors wrote.
Notably, in almost half of the patients who had amputations within 90 days of discharge for CLI, an invasive vascular procedure had not been attempted. Further, rates of revascularization varied substantially between facilities, from a low of 13% to a high of 53%, with a difference in case-mix accounting for just 8% of the variance.
“In a sensitivity analysis, we found that surgical and endovascular capabilities were present in most of the VA facilities during the study period, so lack of such services probably does not fully explain such variability,” Mentias noted. “Further studies are needed to explore the real reason for the variability in revascularization utilization.”
The authors suggested that the presence of extensive tissue necrosis or underlying infection could have driven the amputation-first approach in some patients. Comorbidities could also have been a factor.
“Patients not receiving revascularization had higher prevalence of black race, diabetes mellitus, kidney disease, and heart failure compared with patients who underwent revascularization,” the authors reported.
It seemed likely that other factors played into the significant underutilization of revascularization, however.
“Given the strong association of revascularization with patient outcomes, the above findings highlight an urgent need to develop processes for ensuring that patients with CLIs receive care from specialists with expertise in CLI management,” they concluded.
Statin Use Improved
In addition to revascularization for CLI, guidelines also give a class I recommendation to the use of statins.
“Statin is an important medication in patients with advanced atherosclerotic vascular disease such as CLI. It has been shown consistently to reduce mortality in prior studies,” Mentias said.
During the study period, prescriptions for statins at discharge rose from 47.4% to 60.9%. “However, a big portion of CLI patients (around 40%) still were discharged and were not prescribed any statin within 30 days of discharge,” he added. “So there is room for improvement.”
The study looked at data through 2014, leaving some question as to the current use of both revascularization and statins in this high-risk population.
“It is difficult to extrapolate our results to the following years,” Mentias noted, “especially after introduction of the Veterans’ Choice Act in 2014, which aimed to improve the access of Veterans to medical services in Veterans’ hospitals as well as civilian hospitals.
-
Mentias A, Qazi A, McCoy K, Wallace R, Vaughan-Sarrazin M, Girotra S. Trends in Hospitalization, Management, and Clinical Outcomes Among Veterans With Critical Limb Ischemia. Circ Cardiovasc Interv. 2020;13(2):e008597. doi:10.1161/CIRCINTERVENTIONS.119.008597