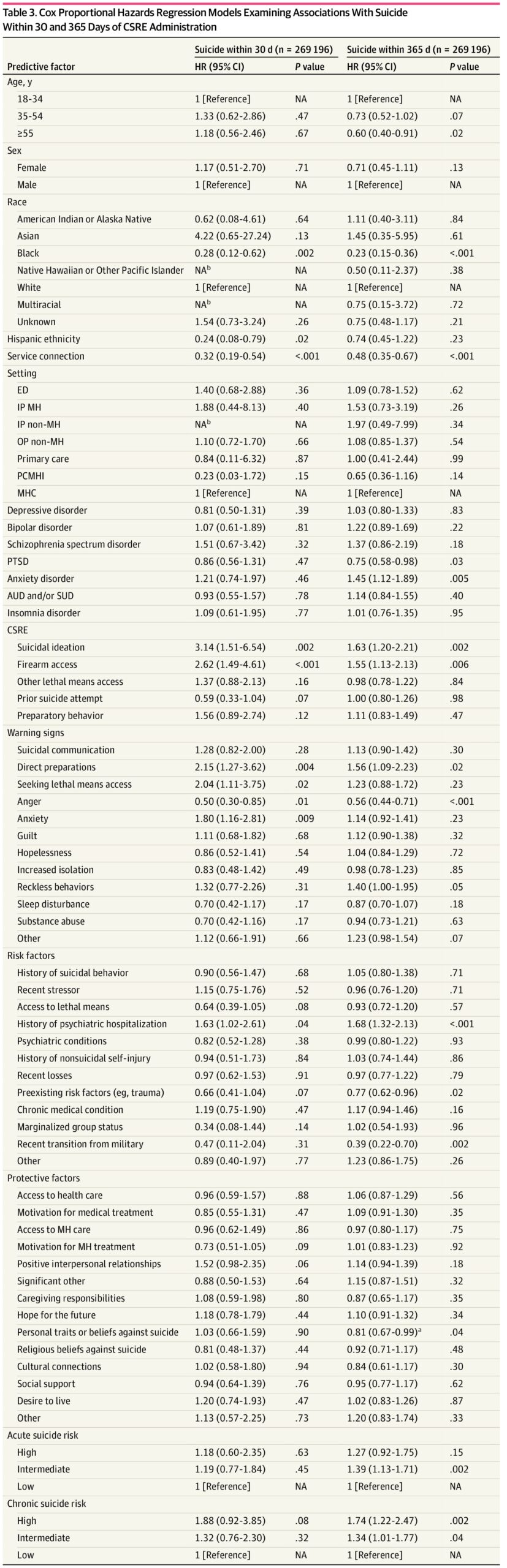
Click to Enlarge: Cox Proportional Hazards Regression Models Examining Associations With Suicide Within 30 and 365 Days of CSRE AdministrationAbbreviations: AUD, alcohol use disorder; CSRE, comprehensive suicide risk evaluation; ED, emergency department; HR, hazard ratio; IP, inpatient; MH, mental health; MHC, mental health clinic; NA, not applicable; OP, outpatient; PCMHI, primary care–mental health integration; PTSD, posttraumatic stress disorder; SUD, substance use disorder.
a. Effect did not meet criteria for being statistically and clinically significant (ie, HR ≤0.77 or ≥1.30 [P ≤ .05]).
b. Effect estimates based on cell sizes of less than 10 patients are suppressed per privacy guidelines. Source: JAMA Network Open
The cohort study published in JAMA Network Open aimed to identify elements of the nationally standardized VHA Comprehensive Suicide Risk Evaluation (CSRE) that are associated with subsequent suicide.1
In U.S. veterans, the age- and sex-adjusted suicide rate increased by 76.3% from 2001 to 2021. The VHA implemented the CSRE in 2019 to standardize suicide risk assessment across the healthcare system. Identifying CSRE responses associated with suicide could inform risk management and prevent suicide, the researchers explained.
The study authors are affiliated with the University of Michigan, Ann Arbor (MI) VAHS, VA Serious Mental Illness Treatment Resource and Evaluation Center in the Office of Mental Health and VA Center for Clinical Management Research in Health Systems Research, each in Ann Arbor, MI. Additional authors are affiliated with the VA Rocky Mountain Mental Illness Research, Education, and Clinical Center for Suicide Prevention and the Anschutz Medical Campus at the University of Colorado, both in Aurora, CO.
“VA has made suicide prevention its top clinical priority. As part of efforts to prevent veteran suicide, VA implemented a standard approach to screen and comprehensively evaluate patients for suicide risk,” Kevin Saulnier, PhD, assistant professor in the Department of Psychiatry at University of Michigan, told U.S. Medicine. “We wanted to understand which risk factors in the tool VA implemented nationally to assist clinicians in evaluating suicide risk were associated with subsequent suicide. Our hope is that this work can inform care for at-risk patients.”
This study examined suicide risk, both acute (within 30 days) and chronic (within 365 days), after 269,374 CSREs were administered to VHA patients undergoing CSRE evaluation between Nov. 1, 2019, and Dec. 31, 2020. The 153,736 total patients were 86.26% male with a mean age of 50.48 years old. Data collection and analysis were performed from April 5, 2024 to Aug. 20, 2024, the study reported.
The investigators used the VHA Corporate Data Warehouse to find demographic and clinical information and the VA-DoD Mortality Data Repository to obtain vital status and cause of death.
“We found that a small subset of responses included in the CSRE were associated with subsequent suicide,” Saulnier said. “In particular, suicidal ideation, firearm access, making preparations for a suicide attempt and a history of psychiatric hospitalization were associated with increased risk for suicide across the statistical models we generated that looked at suicide within 30 and 365 days of the CSRE. Unexpectedly, anger was associated with decreased risk across models.”
This study highlighted risk factors, like firearm access, that may be of particular importance to consider during suicide risk assessments. Determining access and preparation to use lethal means are of the utmost importance, Saulnier pointed out.
“Suicide prediction has long been a challenge for the field,” Saulnier said. “The finding that evaluations conducted in VA are predictive of subsequent suicide highlights the critical role that VA providers are playing in preventing veteran suicide.”
The researchers also found that in adjusted models, no protective factors, such as hope and social support, in the CSRE were associated with acute or chronic suicide risk.
Of the 791 suicides in the 365 days following a CSRE, 144 occurred within 30 days (18.20%). Increased suicide risk within 30 days of CSRE administration was found for CSREs with suicidal ideation, firearm access, direct preparations for a suicide attempt, seeking access to lethal means, anxiety and history of psychiatric hospitalization. Anger was associated with decreased suicide risk within 30 days of CSRE administration, according to the investigators.
The authors suggest that VHA clinicians would benefit from focusing on a subset of CSRE responses. Also, developing risk prediction algorithms may enhance clinical evaluations of suicide risk.
The research team noted the CSRE was developed to include evidence-based factors associated with suicide. This tool identifies constructs for clinicians to use during suicide risk assessments and includes five suicidal ideation, behavior, and lethal means items (i.e., suicidal ideation, firearm access, nonfirearm lethal means access, prior suicide attempts, preparatory behavior), as well as 12 warning signs (e.g., hopelessness), 12 risk factors (e.g., recent losses) and 14 protective factors (e.g., social support).
Although training materials are available, the CSRE isn’t a structured interview and doesn’t include question prompts. CSRE items are scored on a binary presence or absence scale, with suicide-related items also including an option of unknown (combined with absence for these analyses). Using clinical judgment, clinicians place patients in low-, intermediate-, and high-risk strata for acute and chronic suicide risk. CSRE responses are stored as health factors in the Corporate Data Warehouse, the researchers explained.
The study authors concluded that identifying CSRE responses associated with subsequent suicide could provide information about evidence-based suicide risk determinations. Also, establishing the incremental value of the CSRE after taking demographic and diagnostic risk factors into account could inform current practices.
Unexpected findings of the study include decreased chronic suicide risk for patients with anger, preexisting risk factors and a recent transition from the military, the investigators reported.
- Saulnier KG, Bagge CL, Ganoczy D, Bahraini NH, Jagusch J, Hosanagar A, Ilgen MA, Pfeiffer PN. Suicide Risk Evaluations and Suicide in the Veterans Health Administration. JAMA Netw Open. 2025 Feb 3;8(2):e2461559. doi: 10.1001/jamanetworkopen.2024.61559. PMID: 39998832; PMCID: PMC11862973.


