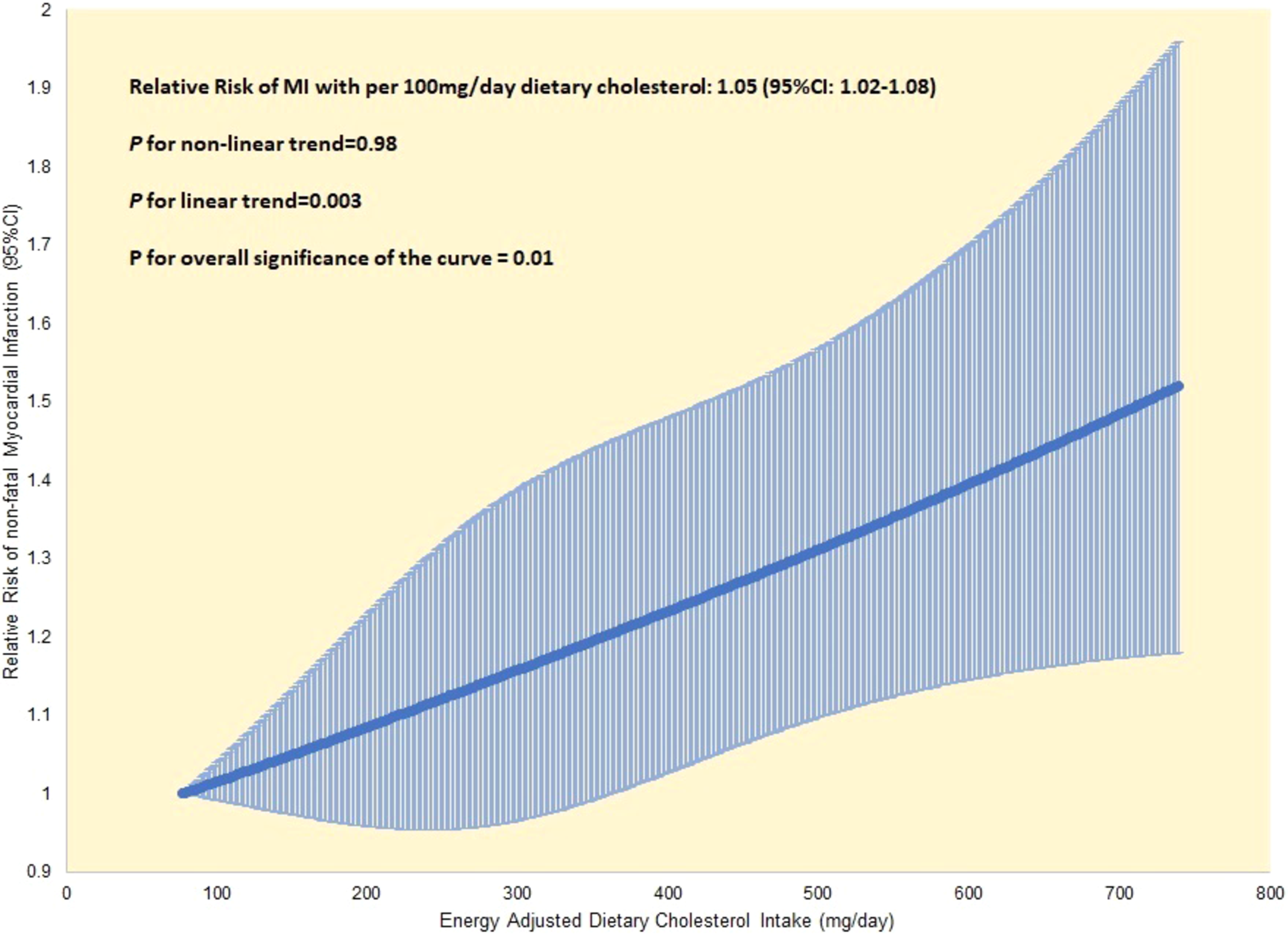
Click to Enlarge: Dose–response relationship between dietary cholesterol intake and risk of MI in the VA Million Veteran Program. Adjusted for age, sex, family history of heart disease, smoking status, total physical activity, body mass index, alcohol intake, total calorie intake, cholesterol‐lowering diet and current cholesterol‐lowering medication use, and baseline history of diabetes, hypertension, and high cholesterol. MI indicates myocardial infarction; and VA, Department of Veterans Affairs. Source: JAMA Network Open
BOSTON — Veterans with a higher dietary intake of cholesterol are at increased risk of having a heart attack, according to a recent study that shows a direct link between dietary cholesterol intake and heart attack risk.
The study published in the Journal of the American Heart Association examined the relation of dietary cholesterol with the incidence of myocardial infarction, also known as heart attack, among participants of the Million Veteran Program (MVP).1
The study authors are affiliated with the Boston and Atlanta VA Healthcare Systems.
Coronary artery disease, a leading cause of morbidity and mortality in the United States, can lead to major complications, including myocardial infarction. Each year in the United States, there are 605,000 new cases of coronary artery disease and 200,000 recurrent cases. Nearly 1 in 4 Americans, or 659,000 individuals, die from heart disease, costing the U.S. medical system $363 billion for healthcare and medication costs, the study reported.
The researchers wanted to study the association between dietary cholesterol intake and the risk of myocardial infarction among MVP participants, because there have been few studies on diet among veterans.
“The Million Veteran Program is one of the largest studies and collects detailed diet information from about half a million veterans,” said Michael Gaziano, MD, executive director of the Massachusetts Veterans Epidemiology Research and Information Collaborative (MAVERIC) at VA Boston Healthcare System and principal investigator of the Million Veteran Program. “This gives us the opportunity to explore the relationships between diet and factors like exercise, weight and genetics and how these affect health and disease.”
This study included 180,156 veterans in the MVP, with a mean follow-up of 3.5 years. Veterans enrolled in the MVP, a nationally representative, prospective cohort study of veterans designed to investigate genetic and nongenetic determinants of chronic diseases, receive routine primary care in the VAHS.
The mean age of study participants across all cholesterol categories was 62 years old, with 90% of participants identifying as men and 80% identifying as white. Veterans were excluded if they had a history of cancer or cardiovascular disease, responded to the MVP Lifestyle Survey after December 2018, didn’t provide dietary information or reported implausible dietary intakes. The researchers analyzed data on relevant dietary intake and evaluated the association between dietary cholesterol and heart-attack risk using statistical analysis.
Dietary-food intake was collected by a self‐reported food-frequency questionnaire, which asked how often a standard portion of each of 61 food items was consumed in the past year. Responses included never or less than once per month, 1 to 3 per month, once a week, 2 to 4 per week, 5 to 6 per week, once a day, 2 to 3 per day, 4 to 5 per day, and greater than 6 per day. Overall dietary quality was estimated with the Dietary Approaches to Stopping Hypertension (DASH) score based on the following eight components: fruits, vegetables, nuts and legumes, low‐fat dairy products, whole grain, sweetened beverages, sodium and red and processed meats. The major food sources that contributed to dietary cholesterol intake based on the questionnaire were eggs, chicken or turkey and beef, pork or lamb as a main dish, according to the researchers.
“Our study found a direct correlation between dietary cholesterol intake and heart attack risk,” Gaziano told U.S. Medicine. “In a straight-line fashion, the higher the dietary intake of cholesterol, the higher the risk of a heart attack. That risk rises by about 5% for every 100 mg/day of cholesterol. For context, the average intake of cholesterol among Americans is approximately 300 mg/day.”
The authors determined that subjects consuming more than 300 mg/day of cholesterol had a 15% increased heart attack risk compared with those consuming less. Cholesterol intake among veterans was mainly attributed to a high consumption of meat and eggs.
Poor adherence to the DASH diet (i.e., a DASH score in the lower 60%) and high dietary cholesterol intake (i.e., 300 mg/day) were independently associated with a higher risk of heart attack. Independently, each factor was associated with about a 20% higher risk of heart attack. Together, both factors were associated with a 36% higher risk, the investigators pointed out.
“The key message for veterans is that your diet is critically important to your overall health,” Gaziano explained. “Diet is one of the eight essential factors for health, according to guidelines from the American Heart Association. Veterans can improve their health by improving diet, getting exercise and refraining from smoking and other harmful habits. Other factors include sleep, weight management, cholesterol management, blood sugar and blood pressure.”
The study also found that, on average, increased dietary cholesterol intake was associated with decreased frequency of vigorous exercise.
For healthcare professionals monitoring dietary cholesterol intake and trying to prevent myocardial infarction in their veteran and military personnel patients, Gaziano acknowledged that providers aren’t always able to conduct a careful assessment of diet for their patients.
“This study reinforces the importance of dietary recommendations and the need to reduce high-cholesterol foods,” Gaziano said. “We aim to integrate a dietary-assessment tool into clinical settings so we can more easily assess diet, exercise and other lifestyle factors. Between data from the MVP … and from individual questionnaires, we hope this will help providers ensure veterans are fully informed as to how to prevent certain cardiovascular ailments.”
The researchers concluded that veterans may reduce the risk of heart attack through lifestyle modification, including dietary changes aligned with the DASH diet and reductions in cholesterol intake, which can be achieved by decreasing the intake of meat and eggs.
This study had several strengths, including a prospective cohort design with a large sample size. Also, participants had diverse socioeconomic backgrounds. A limitation of the study is the use of survey data can be influenced by response bias. In addition, the study has limited generalizability to the overall U.S. population because the study population consisted primarily of men and white subjects, the authors explained.
Gaziano noted the MVP has received major investments in time and effort and serves as a resource to better understand the effect of diet on the health of veterans.
“Future research will explore how other behaviors as well as genes work with diet to affect health and disease,” he said.
- Nguyen XT, Li Y, Nyaeme MS, Panigrahy N, et. Al. VA Million Veteran Program. Dietary Cholesterol and Myocardial Infarction in the Million Veteran Program. J Am Heart Assoc. 2025 Feb 18;14(4):e036819. doi: 10.1161/JAHA.124.036819. Epub 2025 Feb 8. PMID: 39921525.


