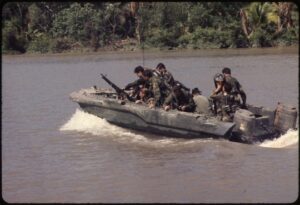
Members of U.S. Navy Seal Team One move down the Bassac River in a Seal team Assault Boat (STAB) during operations along the river south of Saigon in 1967. U.S. Navy photo
NEW YORK — More than a half-century after the United States escalated involvement in the Vietnam War by sending significant combat troops, veterans still face significant psychological and physical health challenges related to their employment.
Those findings come from two major new studies from the Columbia University Mailman School of Public Health and the VA Boston Healthcare System.1,2
For the 35-year-long investigation into the health and well-being of now-aging Vietnam War veterans, average age 72, researchers focused on a subgroup of 729 still-living veterans deployed to Vietnam, drawn from a broader sample of 12,400 men who served in the U.S. armed forces during the Vietnam War. The participants were surveyed over three data collection periods—1984, 1998 and 2020—revealing that both combat exposure and PTSD are key predictors of long-term physical and mental health outcomes.
“Combat exposure and PTSD were strong predictors of heart disease and other chronic illnesses in veterans, especially those who faced the most intense combat,” explained Jeanne Stellman, PhD, co-author and professor emerita of health policy and management at Columbia Mailman School. “This research reinforces how the trauma of war continues to affect veterans long after the war ends.”
The study’s findings are especially concerning regarding veterans’ cardiovascular health: 28% of participants reported being diagnosed with heart disease, with those who experienced higher levels of combat exposure being twice as likely to report heart disease compared to those with less exposure. PTSD also was strongly associated with increased rates of chronic conditions such as arthritis (46.5%), sleep apnea (33%) and gastroesophageal reflux disease (GERD) (23.5%).
“These findings are significant not only for veterans but for public health as a whole,” said Steven Stellman, PhD, co-author and professor emeritus of epidemiology at Columbia Mailman. “The ongoing health risks, particularly cardiovascular disease, highlight the need for long-term care strategies that account for both the psychological and physical burdens of PTSD.”
Four PTSD patterns emerged over 35 years:
- current PTSD (9.1%, rising to 15.5% in heavy combat),
- prior PTSD (9.7%),
- sub-threshold PTSD (25.2%) and
- never PTSD (56.0%).
Worse Outcomes
“A strong combat-PTSD dose-response relationship persisted across timepoints,” the authors explained. “Veterans with current PTSD showed the worst outcomes; those with sub-threshold or prior PTSD had intermediate outcomes, while never-PTSD veterans fared best. Community support mitigated adverse effects.”
It was especially significant to find related dysfunction affecting veterans even below clinical thresholds, leaving many ineligible for VA programs. The article explained that a form of PTSD where veterans’ symptoms fall below the threshold for a formal diagnosis was identified as a significant contributor to health issues. Veterans with sub-threshold PTSD were found to have worse physical and mental health outcomes than those who never experienced PTSD.
“Veterans with sub-threshold PTSD suffer significant health burdens that are often overlooked,” said Steven Stellman, emphasizing the need for updated VA policies to include these veterans in care and treatment programs.
The studies identified combat and combat-related PTSD as risk factors for heart disease and noncardiac chronic disease comorbidity in deployed Vietnam veterans. The data came from a random sample of 735 Vietnam-deployed American Legionnaires who were surveyed in 1984, 1998 and 2000 for combat exposure, probable PTSD and history of diagnosed chronic illnesses.
Of those, 28% reported a diagnosed heart condition, and combat exposure in Vietnam was a significant predictor (OR = 1.92, 95% confidence interval 1.13-3.31). Furthermore, veterans with heart disease reported significantly more comorbid chronic illnesses, including arthritis and respiratory conditions: sleep apnea, emphysema and asthma. Chronic illnesses were reported even more often by men with PTSD.
Emerging evidence suggests that, 50 years after Vietnam, combat and associated PTSD may contribute to heart disease and comorbid conditions.
Those with PTSD or sub-threshold PTSD reported significantly worse life satisfaction, higher levels of anxiety and depression and poorer overall health, according to the researchers, who also linked PTSD to social and familial challenges.
Veterans with PTSD or sub-threshold PTSD were found to have higher rates of divorce and separation, especially those who had been exposed to more intense combat.
“The relationship between PTSD and chronic illness, particularly cardiovascular disease, continues to evolve, and it is essential to continue assessing and treating the long-term effects of these conditions,” said Jeanne Stellman. “This study provides crucial insights into the lasting legacy of the Vietnam War on those who served and underscores the urgent need for improved care and policies to address their ongoing health needs.”
- Stellman SD, Kaiser AP, Smith BN, Spiro A, Stellman JM. Impact of Persistent Combat-Related PTSD on Heart Disease and Chronic Disease Comorbidity in Aging Vietnam Veterans. J Occup Environ Med. 2024 Dec 18. doi: 10.1097/JOM.0000000000003302. Epub ahead of print. PMID: 39696828.
- Stellman, SD, Pless A, Smith BN, Spiro A, Stellman JM. Persistence and Patterns of Combat-Related PTSD, Medical, and Social Dysfunction in Male Military Veterans 50 Years After Deployment to Vietnam. Journal of Occupational and Environmental Medicine. ():10.1097/JOM.0000000000003321, January 21, 2025. | DOI: 10.1097/JOM.0000000000003321

