NASHVILLE — More than 30 million U.S. adults—including approximately 25% of veterans—have diabetes, putting them at increased risk of heart disease. Clinical trials have demonstrated that sodium-glucose cotransporter 2 inhibitors (SGLT2is), an emerging and essential class of medications for treating Type 2 diabetes, can significantly reduce major adverse cardiovascular events. However, some studies have also suggested a potential downside—an increased incidence of peripheral arterial disease (PAD)-related surgical procedures, including amputations.
A new study in Diabetes Care sought to examine this association in a large cohort of veterans.1
PAD is a condition in which arteries narrowed by atherosclerosis restrict blood flow to the limbs, typically the legs. This reduced circulation increases the risk of heart attack, stroke, and, in severe cases, amputation. “There are a large number of veterans with diabetes who are at high risk for peripheral artery disease due to multiple risk factors including heart disease, longer durations of diabetes and a high prevalence of current and former tobacco users,” said Christianne L. Roumie, MD, MPH, corresponding author of the study.
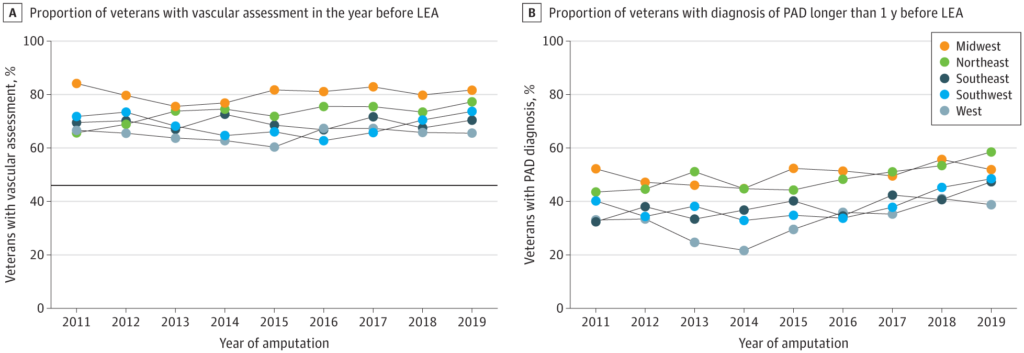
Click to Enlarge: Proportion of Veterans With Vascular Assessment and Peripheral Artery Disease (PAD) Diagnosis by Region and Year From 2001 to 2019A, Black, horizontal line represents the proportion of individuals who had vascular assessment in the private sector from a previous study. LEA indicates lower extremity amputation. Source: JAMA Network
The retrospective cohort study analyzed veterans age 18 and older with diabetes who received care from the VHA between Oct, 1, 2000, and Dec. 31, 2021. “We collected veterans’ routine care and comorbid conditions and accounted for those, as well as their duration of diabetes,” said Roumie, professor of internal medicine and pediatrics at Vanderbilt University Medical Center and director of VETWISE-LHS Center of Innovation, VA Tennessee Valley Healthcare System. “Patients needed to continue on the diabetes medications, and we measured their refills at the VA pharmacies or prescriptions paid for by Medicare as a measure of medication persistence that was required during the follow-up time.”
The study evaluated new use of SGLT2i or DPP-4i medications as an add-on to metformin, sulfonylurea or insulin treatment—alone or in combination—to determine their association with PAD-related surgical procedures, including peripheral revascularization and amputation.1
The use of DPP-4 inhibitors as a comparator addressed a key knowledge gap, Roumie explained. “Many newer diabetes medications were tested versus a placebo, making it difficult to know if one type offers an advantage over another,” she said. “We wanted to see if there were differences in events when comparing commonly used drug classes. DPP-4 inhibitors are regarded as neutral with respect to cardiovascular events and are widely used.”
The study cohort included 76,072 SGLT2i use episodes and 75,833 DPP-4i use episodes. Key characteristics of the cohort included a median age of 69 years, a median HbA1c of 8.4% and a median diabetes duration of 10.1 years.
Results showed that PAD events occurred at a rate of 11.2 per 1,000 person-years among SGLT2i users, compared to 10.0 per 1,000 person-years among DPP-4i users. The adjusted hazard ratio (aHR) for PAD events associated with SGLT2i use was 1.18 (95% CI 1.08-1.29), indicating an 18% increased risk of PAD-related surgical procedures compared to DPP-4i users. Notably, this increased risk persisted when events were tracked up to 360 days after SGLT2i discontinuation.
“The association of SGLT2i on peripheral revascularization and amputation was seen in all subgroups that were examined, including those with and without prior diagnosis of osteomyelitis, as well as those who used insulin and those who did not,” Roumie told U.S. Medicine. “But in some cases, confidence intervals were wide because of smaller subgroup size.”
While the mechanism linking SGLT2i use to worsening PAD and amputations remains unclear, Roumie noted that several theories exist. “It has been speculated that the increased risk of amputations is due to the progression of arteriosclerosis, which negatively impacts perfusion. Others have suggested that hemodynamic instability occurs during the early stages of SGLT2i use, contributing to intravascular damage,” she said.
Given the conflicting findings between clinical trials and observational studies, an expert panel reviewed available clinical trial data through 2019, she said. “They concluded that amputation risk increased with canagliflozin only and was not an SGLT2i class effect. However, the panel acknowledged that more data are needed.”
Roumie emphasized that, as with all medications, the benefits of SGLT2i must be carefully weighed against potential risks. “Clinicians can choose to conduct a risk-stratified approach for high-risk patients using additional peripheral vascular testing,” she said. “We believe that this information can be incorporated into future guidelines and can guide clinicians to a more tailored approach to prescribing diabetes regimens that would maximize patient benefits and minimize the potential for adverse side effects.”
- Griffin KE, Snyder K, Javid AH, Hackstadt A, Greevy R, Grijalva CG, Roumie CL. Use of SGLT2i Versus DPP-4i as an Add-On Therapy and the Risk of Peripheral Artery Disease Surgeries. Diabetes Care. 2024. doi:10.2337/dc24-1546.
