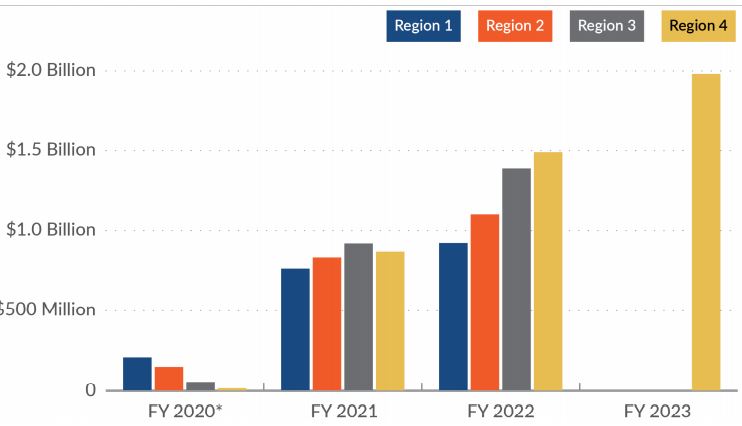
Click to Enlarge: VHA outpatient claim payments to Optum for CCN regions 1–3, FY 2020 through FY 2022 and to TriWest for CCN region 4, FY 2020 through FY 2023.
Source: Community Care Reimbursement System payment data from the Program Integrity Tool for Optum
from FY 2020 (quarter 1) through FY 2022 (quarter 4) and from the Corporate Data Warehouse for TriWest
from FY 2020 (quarter 4) through FY 2023 (quarter 4).
* Full implementation dates for the CCN contracts varied by region from FY 2020 through FY 2022. For
region 5, outpatient claim payments to TriWest totaled about $100.4 million through FY 2023.
WASHINGTON, DC — As promised, the new Republican-led Congress began the legislative year by focusing heavily on community care in VA, with a glut of hearings targeting different aspects of the issue.
While the message from Republicans was that “community care is VA care” and access needs to be expanded, Democrats maintained that the expansion comes at the expense of direct care, the quality of which can be guaranteed in a way that care in the community cannot.
“There will always be a place for community care. VA cannot provide all the care veterans need on its own,” Rep. Julia Brownley (D-CA) said at a House VA Oversight Subcommittee hearing on the topic. “Finding the right balance is important, and I’m concerned we have not yet found that balance. … There are a number of weaknesses in VA’s oversight of the performance of its third-party [community care administrators]. … Worse still, we don’t even know if patients referred to the community are receiving more timely access to care or even high-quality care, because VA has not established sufficient contractual requirements and metrics.”
Oversight agencies were on hand to testify to the flaws in the community care system. According to Government Accountability Office (GAO) officials, the agency has made 27 recommendations to VA since the implementation of the Veterans Community Care Program in 2018, only 9 of which have been fully implemented.
“VA has still not fully implemented our 2018 recommendation to implement a timelines standard for community providers,” testified Sharon Silas, GAO’s director of health care. “Without a complete picture of how long it takes a veteran to complete care, whether it’s through the VA or a community provider, it will be difficult for VA to know whether it’s achieving its goal of timely access to care.”
GAO also has provided recommendations for shoring up the adequacy of VA’s community care network, which their reports have called into question.
“In our 2024 report, we found that VA’s methodology to calculate [whether a network is sufficient] does not include all the claims in their calculations. This raises concerns as to whether VA is fully accessing the adequacy of [its networks],” Silas said.
The other primary VA watchdog, VA’s Office of the Inspector General, has issued 50 reports focusing on community care over the past five years and has found several consistent problems, explained Principal Deputy Assistant IG Julie Kroviak. The most concerning is that VA cannot ensure the seamlessness or adequacy of community care.
“The community care program lacks robust quality assurance policies,” Kroviak said. “When VA providers cannot even get timely access to basic clinical documentation detailing a community provider’s management of a referred veteran, any opportunity to monitor that care quality is lost.”
Exacerbating these issues is a lack of communication between VA and community providers. VA records do not always transfer to community providers, and those providers do not always send patient records back to the VA. The result can be a disjointed care experience for veterans.
Solutions to some of these issues will require new contracts with the third-party administrators overseeing VA’s networks. The new contracts could include provisions for tracking quality and timeliness, as well as ensuring that community providers are properly trained in veteran care, like screening for PTSD, TBI and military sexual trauma.
However, legislators were informed last month that VA does not expect to award the next generation of community care contracts until summer of 2027.
“As we are going through the requirements process to identify what needs to be in these contracts, we want to make sure they’re done according to acquisition standards,” explained VHA’s Chief Operating Officer Steven Braverman. “[The summer 2027 timeline] is based on us committing to moving as quickly as possible to making those decisions.”
“Since the [PACT Act] took effect, nearly 900,000 veterans have enrolled in VA care, with even more moving into higher priority groups, in part because of an increase in service disability ratings,” Braverman explained. “Corresponding elimination of copays and increased eligibility for medical services have led to more reliance on VA care that can’t be met in the direct care system alone. I can confidently say we can’t meet veteran demand without the partnership and collaboration of third-party administrators and community providers.”

