Health Literacy Is a Factor
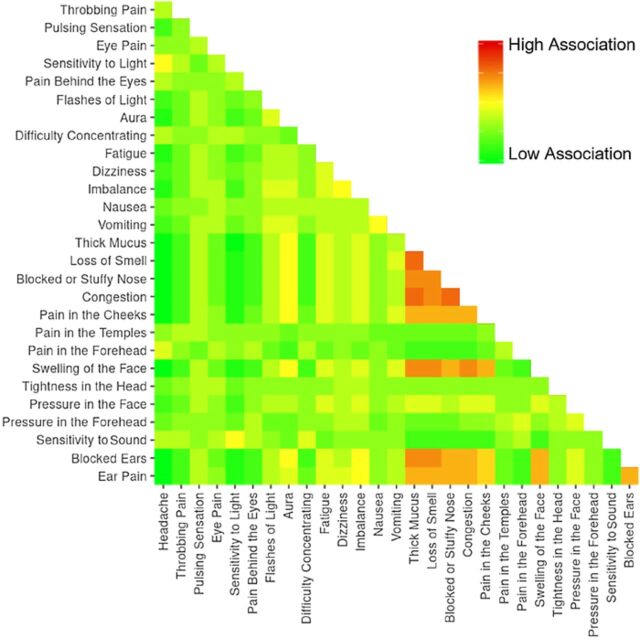
Click to Enlarge: Heat map displaying the associations of individual symptom terms. Source: National Library of Medicine
BETHESDA, MD — Headaches are an almost universal experience, affecting approximately 96% of people globally at some point in their lives. Migraines, with a lifetime prevalence of 12.9% to 15.2%, consistently rank among the top three leading causes of disability for both men and women. Yet, despite guidelines that define clear diagnostic criteria for migraines and several migraine subtypes, diagnosis remains difficult.
Up to 53% of patients experience a delay from symptom onset to diagnosis of more than 5 years—a delay which a new study attributes in part to a phenomenon known as health literacy.
“Health literacy is the extent to which patients understand and interpret information provided by their healthcare professionals,” stated the authors of the study published in the Ochsner Journal. “While otolaryngology patients appear to have high levels of health literacy, the definitions of otolaryngologic complaints such as congestion, dizziness, sinus infections and reflux have substantial variability between patients and clinicians.”
To investigate potential differences between patients and otolaryngology providers in defining the symptoms related to migraine researchers asked patients and otolaryngology providers at five academic medical centers across the United States—Walter Reed National Military Medical Center, Bethesda, MD; Tulane University, New Orleans; University of Washington, Seattle; Albert Einstein College of Medicine, Bronx, NY; and Washington University School of Medicine, St. Louis—to select as many symptoms as they felt were related to migraine from a list of 28 common symptom terms.
For the purpose of the analysis, the symptoms were grouped into six broad domains: headache-related symptoms (headache, throbbing pain, pulsing sensation), eye-related symptoms (eye pain, sensitivity to light, pain behind eyes, flashes of light, aura), systemic symptoms (difficulty concentrating, fatigue, dizziness, imbalance, nausea, vomiting), sinonasal symptoms (thick mucus, loss of smell, blocked or stuffy nose, congestion), facial symptoms (pain in the cheeks, pain in the temples, pain in the forehead, swelling of the face, tightness in the head, pressure in the face, pressure in the forehead) and ear-related symptoms (sensitivity to sound, blocked ears, ear pain). Patients and clinicians selected a similar number of symptoms (a median of 10 and 11, collectively).
Participating were 381 patients and 31 otolaryngology clinicians across the medical centers’ five geographic regions.
Key Differences
The findings: Patients and clinicians selected a similar number of symptoms (a median of 10 and 11 collectively). However, the types of symptoms the two groups associated with migraines had some key differences.
Patients most often defined migraine using headache-related symptoms (94.2%), followed by eye-related symptoms (89.5%) and facial symptoms (85.0%). At least half of patients associated migraine with the specific symptoms of headache (87.4%), sensitivity to light (77.4%), pain behind eyes (63.3%), throbbing pain (62.2%), sensitivity to sound (62.2%), pain in the forehead (61.4%), difficulty concentrating (59.3%), pain in the temples (54.6%) and eye pain (50.1%). Otolaryngologists, on the other hand, were more likely to define migraine using symptoms from the eye-related and ear-related domains.
Within the symptom domains for which patients and providers demonstrated no overall difference in response rates (headache-related, systemic and sinonasal), clinicians were more likely to select three individual symptoms to define migraine: nausea, vomiting and headache. The single largest discrepancy was in the symptom of aura, that providers selected 63.7% more often than patients.
The researchers also investigated whether geographic location influenced patients’ perception of migraine symptoms and found no significant overall impact, though a few notable differences were observed: Patients from New Orleans were twice as likely as those from Washington, DC, to define migraine using facial symptoms and were only half as likely to define migraine using eye-related symptoms. Systemic symptoms were more likely to be selected by patients in Washington, DC and New York, New Orleans, LA or St. Louis. In contrast, headache-related, sinonasal and ear-related symptoms were relatively consistent independent of geographic location.
“Semantic differences may exist for several reasons such as education level, exposure to medical care, and insurance status, but overall, these differences highlight reasons communication may be limited and can negatively impact the patient-provider relationship,” wrote Jakob L. Fischer, MD, and his colleagues. Fischer, the study’s first author, conducted the research as a resident at Walter Reed.
Because the diagnosis of migraine relies heavily on patient reporting of subjective symptoms, many patients experience substantial delays in the diagnosis and treatment of migraine, the researchers stated. “This delay in diagnosis may be in part attributable to these differences in interpretation of the symptoms associated with migraine.”
“Understanding migraine and being able to communicate with patients regarding the symptoms associated with migraine is critically important to the otolaryngologist,” they concluded.
- Fischer JL, Tolisano AM, Navarro AI, Abuzeid WM, Humphreys IM, Akbar NA, et al. I’m Getting a Migraine: A Comparative Evaluation of Patient and Clinician Interpretations of Migraine Symptoms. Ochsner J. 2024 Winter;24(4):262-272. doi: 10.31486/toj.24.0071. PMID: 39720823; PMCID: PMC11666111.

