PROVIDENCE, RI — For the first time in more than 50 years, the VA will fund a study on psychedelic-assisted therapy for post-traumatic stress disorder and alcohol-use disorder among veterans.
The potential of methylenedioxymethamphetamine (MDMA)-assisted therapy as a treatment option for veterans with both PTSD and AUD will be evaluated by VA researchers affiliated with Brown University in Providence, RI, and Yale University in New Haven, CT. Participants will receive psychotherapy sessions enhanced by pharmaceutical-grade MDMA, a psychedelic compound believed to increase emotional openness, reduce fear, and promote introspection during therapy. The active placebo received by some randomly-chosen participants will be a lower dose of MDMA.
The study will take place at the Providence and West Haven, CT, VAMCs and is expected to begin enrollment this year. The grant award is approximately $1.5 million over 5 years.
The funding is part of an effort to gather definitive scientific evidence on the potential efficacy and safety of psychedelic compounds such as MDMA and psilocybin when used in conjunction with psychotherapy to treat veterans with PTSD, depression and other related conditions, according to VA officials. “VA is on the cutting edge of clinical research for Veteran health, including in the investigation of psychedelics for mental health,” said Under Secretary for Health Shereef Elnahal, MD. “This study will give us better insight into the potential of MDMA-assisted therapy as a treatment for veterans.”
Psychedelic drugs are a class of substances that alter consciousness or awareness and can be organically or synthetically produced. To prevent serious self-injury or harm, VA strongly discourages self-medicating with psychedelics or any other unprescribed substances and says veterans should always consult their healthcare providers before making any treatment decisions.
A recent review led by VA’s VISN-22 Mental Illness Research Education Clinical Center in Los Angeles noted that neurorehabilitation in military populations “is complicated by higher rates of PTSD and unique characteristics of military institutions. These factors can adversely impact the patient-therapist therapeutic alliance and engagement with the rehabilitation process, leading to poorer outcomes.”
Novel Treatment
The article pointed out that MDMA is a nonclassical psychedelic with pro-social and fear-regulating properties. The researchers noted in the journal NeuroRehabilitation that MDMA-assisted therapy is being explored as a novel treatment for PTSD and potentially could cause rapid symptom improvement and enhance therapeutic alliance.1
Their review of MDMA-assisted therapy for PTSD is provided in the context of neurorehabilitation in military populations, with the authors pointing out, “Results from late-stage clinical trials suggest MDMA-assisted therapy for PTSD would be of particular benefit for military populations with PTSD. The unique pro-social properties of MDMA could be leveraged to enhance the therapeutic alliance and patient engagement during neurorehabilitation.”
The researchers noted the many similarities in patient-therapist dynamics in PTSD treatment and neurorehabilitation, adding, “The properties of MDMA which enhance therapeutic alliance, downregulate fear, and increase cognitive flexibility would potentially benefit both military personnel with and without PTSD undergoing neurorehabilitation.”
Background information in the article pointed out that military personnel undergoing rehabilitation for neurological injury face unique challenges. Those range from context of injury, psychiatric co-morbidities, and the cultural implications of disability during service, they explained. “Neurorehabilitation in this demographic requires unique multidisciplinary considerations to facilitate treatment engagement and achieve optimal recovery outcomes,” they wrote.
One key difference is that neurological injury in military populations tends to occur in the context of physical trauma, such as training or combat, in a young, healthy population. In civilians, cerebral vascular accidents often occur in patients of advanced age who have multiple medical co-morbidities.
“The context and severity of military injuries lends itself to a higher incident of psychological trauma that can manifest as operational stress injury (OSI) or post-traumatic stress disorder (PTSD),” according to the authors. “The presence of PTSD can interfere with the rehabilitation process, leading to poorer neurological and functional outcomes. Therefore, timely and effective treatment of PTSD is essential for successful neurorehabilitation. While there is robust evidence for existing PTSD therapies, there are limitations with high drop-out rates and large proportions of patients do not respond. This has led to the development of alternative therapeutic methods.”
MDMA (3,4-Methylenedioxymethamphetamine) is a non-classical psychedelic with empathogen effects that is being studied for the treatment of PTSD, the researchers reported.
Despite optimism in that study, the Food and Drug Administration declined to approve MDMA-assisted therapy for the treatment of PTSD last year. The FDA said there was insufficient data to allow its use.
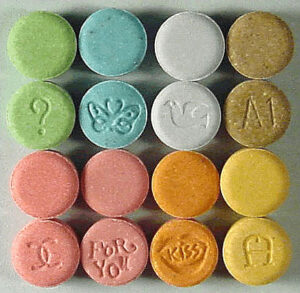
The company seeking approval for the treatment, Lykos Therapeutics, was asked to conduct an additional clinical trial to assess whether the drug, commonly known as Ecstasy or molly, would be safe and effective.
- Dunn W, Bershad A, Krantz DE, Vermetten E. MDMA for treatment of PTSD and neurorehabilitation in military populations. NeuroRehabilitation. 2024;55(3):357-368. doi: 10.3233/NRE-230270. PMID: 39331116; PMCID: PMC11612990.