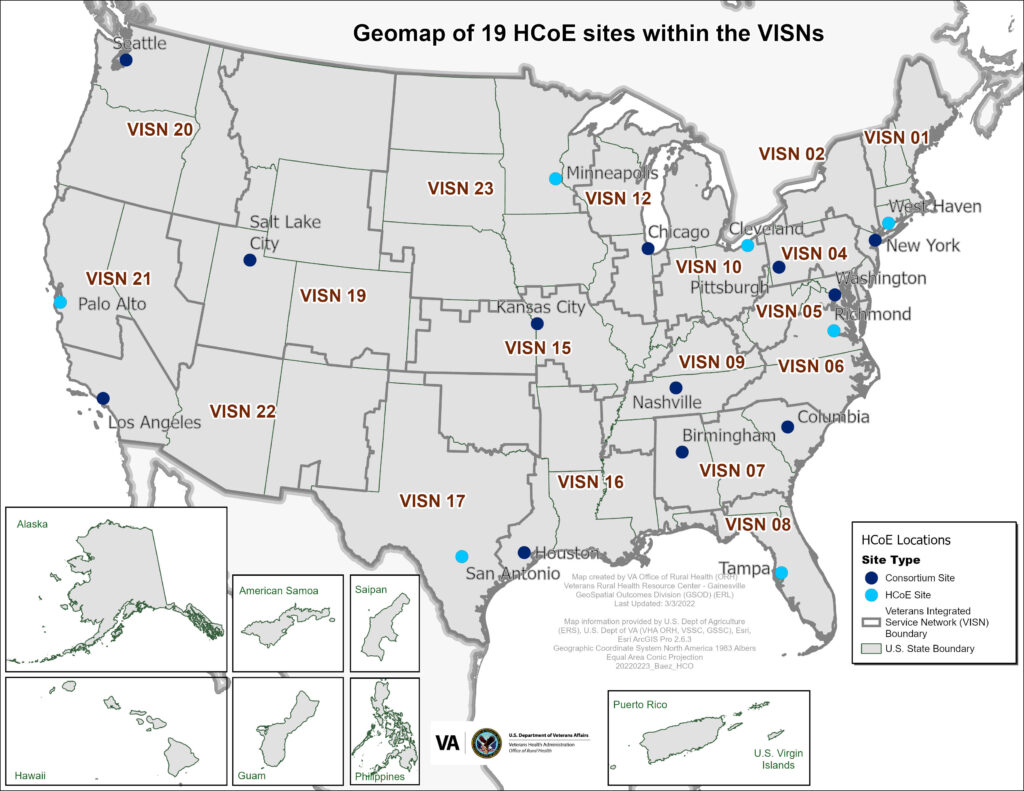
The Headache Centers of Excellence (HCoE) Program, which now has grown to 19 locations, was established by the VHA in 2018. Since 2008, more than 1.74 million veterans have received care within VHA for headache. In fiscal year 2021, nearly 420,000 veterans had at least one appointment with a medical provider in VHA related to headache with more than 25% of the veterans having their first ever appointment for headache in VHA. Source: VA
NEW HAVEN, CT — Expanded recommendations for treatment, preventive therapies and nonpharmacologic therapies are among noteworthy changes in the recently updated VA and Department of Defense (DoD) Clinical Practice Guideline for the Management of Headache.
The guideline, which provides a broad scope of recommendations for the three most common primary headache types and selected secondary headache types, addresses a significant health issue for veterans. Among veterans with a history of TBI, up to 90% experience headaches during the first year after the injury. Chronic daily headaches, defined as headaches occurring 15 or more days per month, are reported in up to 36% of veterans with TBI or PTSD, and migraines affect approximately 20-40% of veterans, depending on the population studied.
The update was performed by a work group of subject experts from the VA and DoD, who developed 12 key questions to guide a systematic search using predefined inclusion and exclusion criteria. After reviewing evidence from five databases published between March 6, 2019, and Aug. 16, 2022, the work group considered the strength and quality of the evidence, patient preferences and benefits versus harms on critical outcomes before making consensus recommendations, which they rated as “strong” or “weak.”
While the guideline is typically updated every 5 years, the latest update was undertaken ahead of schedule because of the rapid expansion and evolution of headache medicine and therapeutics, according to authors of a review of the updated guideline, published in Annals of Internal Medicine. The review, which was led by Jason Sico, MD, MHS, director of research and clinical care, Headache Center of Excellence, Neurology, VA Connecticut Healthcare System, summarizes some of the important updates from the 2020 guideline that are particularly relevant to primary care. They include the following:1
Abortive Therapies for Migraine
The updated guidelines for abortive migraine therapies emphasize early, tailored treatment to alleviate pain and restore function. Recommendations focus on outpatient strategies, considering pain severity, nausea, comorbidities and patient preferences. Aspirin—acetaminophen—caffeine is strongly recommended for its significant benefits and mild adverse effects. Gepants (ubrogepant, rimegepant) are weakly recommended for moderate efficacy, while lasmiditan, effective but with significant adverse effects, received no directional recommendation. Greater occipital nerve blockade remains weakly recommended due to balanced risks and benefits, low evidence quality and practicality in outpatient settings. These updates highlight the need for individualized care based on efficacy, safety and accessibility.
Preventive Therapies for EM or CM
Preventive migraine therapies are recommended for patients with migraines 4 more days a month or 2 or more with significant disability. Episodic migraine (EM) involves fewer than 15 headache days/month, while chronic migraine (CM) involves 15 or more days. Prevention aims to reduce migraine frequency, severity and duration, enhance responsiveness to abortive treatments and decrease medication use.
CGRP monoclonal antibodies (erenumab, fremanezumab, galcanezumab) received strong recommendations for EM and CM, reducing monthly migraine days and abortive medication use. Gepants (atogepant, rimegepant) showed moderate efficacy, with atogepant weakly recommended and rimegepant neutral. Topiramate and valproate received weak recommendations for EM and CM, while gabapentin was discouraged due to inefficacy and misuse risks.
OnabotulinumtoxinA is weakly recommended for CM, but not for EM. Eptinezumab, an intravenous CGRP antagonist, is weakly recommended for EM and CM due to its efficacy and safety, despite logistical challenges. Evidence is insufficient for using greater occipital nerve blocks for CM prevention.
Abortive and Preventive Therapies for TTH
Tension-type headache (TTH) is the most common primary headache. Abortive treatments aim to achieve pain relief, while preventive therapies focus on reducing headache frequency and severity. For acute TTH, ibuprofen (400 mg) or acetaminophen (1,000 mg) is weakly recommended due to significant pain-free responses within two hours. Lower acetaminophen doses were ineffective. Amitriptyline (50-100 mg) is weakly recommended for prevention, significantly reducing monthly headache days but requiring caution due to anticholinergic side effects and overdose risks. OnabotulinumtoxinA showed no significant benefit for chronic TTH and is not recommended.
Nonpharmacologic Therapies for Headache Management
Behavioral medicine interventions such as biofeedback, cognitive behavioral therapy (CBT), mindfulness and progressive muscle relaxation showed mixed or insufficient evidence for standalone use. Rehabilitation interventions, including physical therapy (PT) and aerobic or strength training, received “weak for” recommendations for managing migraines and tension-type headaches (TTH) due to benefits such as reduced headache frequency and intensity. PT techniques included thermal methods, massage and mobilization, while exercise regimens improved vascular and headache control.
Neuromodulation, using electrical or magnetic stimulation to regulate neural pathways, lacked sufficient evidence for acute or preventive migraine treatment. Clinicians should consider contraindications and treatment-specific protocols when exploring these options, the guidelines advise.
Comparisons With Other Guidelines
Although the guideline differs in scope and development from those of the American Academy of Neurology (AAN) and American Headache Society (AHS), which typically encompass a singular headache type, there are many consistent messages, including recommendations for triptans for acute migraines and recommendations for lisinopril, candesartan, topiramate, propranolol and valproate for migraine prevention, according to the reviewers.
But, unlike the updated VA/DoD guideline, the most recent AAN and AHS guidelines for migraine did not discuss CGRP monoclonal antibodies, gepants or lasmiditan, because these pharmacotherapies were only recently approved. “Recommendations related to rehabilitation approaches in the management of migraine, including PT and exercise, are unique to this guideline,” the reviewers wrote.
“This [general practice guideline] provides clinicians with the most up-to-date, evidence-based recommendations available for the evaluation and treatment of headache, combined with tables and algorithms to make the clinically pertinent information easily available,” the reviewers concluded. “Clinicians should work with their patients in crafting treatment plans that account for headache type or types, comorbid conditions, and values and preferences.”
- Sico JJ, Antonovich NM, Ballard-Hernandez J, Buelt AC, et al. 2023 U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline for the Management of Headache. Ann Intern Med. 2024 Oct 29. doi: 10.7326/ANNALS-24-00551. Epub ahead of print. PMID: 39467289.

