Findings Likely to Fuel Debate Over Expansion of Outside Care
WASHINGTON, DC — With the debate heating up about how much VA care should be shifted to the community, a new study found that VA hospitals changed in a 5-year period from 2017 to 2021 from providing worse experiences for Black and poor-health patients to outperforming community hospitals for those and all other patient subgroups examined.
The research is one of a series of studies demonstrating that VA care is superior to community care for a range of conditions or circumstances. That information will fuel the debate over a new bill introduced by House Veterans Affairs Committee Chairman Mike Bost (R-IL). The Complete the Mission Act is a followup to the 2018 Mission Act that then-President Donald Trump signed into law. It expanded veterans’ access to private sector care paid for by the VA. The new bill seeks to ensure existing access standards for private sector “community care” are codified in law, while expanding access to outside services. The VA secretary-designate, former Rep. Doug Collins, (R-GA) has indicated an interest in expanding community care.
The study led by Rand Corp. researchers in Santa Monica, CA, estimated differences in patient experiences for VHA patients compared to non-VA patients in 2017, when there was concern about the health quality of VA hospitals, and in 2021, the second year of the COVID-19 pandemic. The analysis examined the issue, both overall and for specific patient groups.
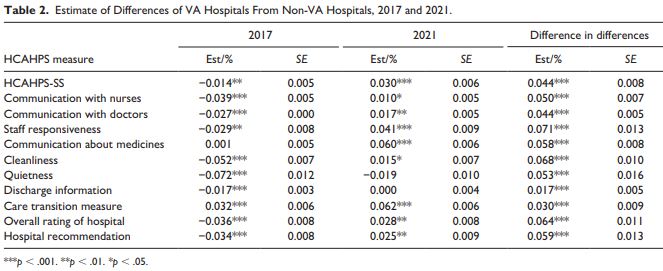
For the report in Medical Care Research & Review, the researchers used data from the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey. They advised that, in 2017, HCAHPS performance was somewhat better for non-VA than for VA hospitals, with Care Transition being the only measure for which VA hospitals performed better on average. But, by 2021, HCAHPS performance was better for VA than for non-VA hospitals for all but two measure—Quietness and Discharge Information—for which there were no differences from non-VA hospitals.1
Since 2006, the Centers for Medicare & Medicaid Services (CMS) has administered the HCAHPS Survey, which provides a standardized survey instrument and data collection methodology for measuring inpatient experiences. That enables valid comparisons to be made across hospitals, according to study authors.
“To enable “apples-to-apples” comparisons to support consumer choice, it was necessary to introduce this standard measurement approach (hcahpsonline.org),” they wrote. “The Veterans Health Administration (VA) is one of the United States’ largest managed care organizations and has been a leader in developing innovative care across settings, including hospitals. Congress, veterans groups, and the media have expressed concerns about access and quality of care in VA settings.”
Originally, the VA collected data on outpatient care experiences through the VA Survey of Health Care Experiences of Patients, which included domains from the Consumer Healthcare Providers and Systems (CAHPS) program. Starting in 2017, the VA began administering HCAHPS, generally following the official HCAHPS protocols.
“Our paper makes two new contributions,” the researchers asserted. “Despite serving a patient population with substantial disease burden, prior research shows that VA hospital quality of care generally compares favorably to non-VA quality of care, although often without specific examination of groups highly represented in VA care. Our first contribution is to examine differences in VA and non-VA hospital experiences for two such groups, the less healthy (vis-à-vis the healthier) and Black patients (vis-à-vis white patients). Our second contribution is that we describe changes in difference in patient experiences for VA compared with non-VA patient groups over time.”
Specifically, the study said it examined differences in 2017 (when the VA Patient Experiences Office initiated activities to improve VA patient experiences nationwide and the VA started following official HCAHPS protocols) and in 2021, the second year of the COVID-19 pandemic.
In the first two years of the COVID-19 pandemic, according to the report, patient experiences in non-VA hospitals declined following an 11-year period of slow but steady improvement but no examination had occurred of the change in VA hospital patients’ experience during the pandemic.
“In contrast to 2017, in 2021 VA hospitals provided better patient care experiences than non-VA hospitals overall, for all HCAHPS measures and for all patient groups assessed,” the study team advised. “The degree of improvement in VA hospitals over 4 years is remarkable under any circumstances, but especially since this period included the first 2 years of the COVID-19 pandemic, during which the performance of non-VA hospitals declined.”
The finding that patients reported overall worse experiences in VA versus non-VA hospitals in 2017 is in line with prior findings. For example, one study found that in 2014, VA hospitals scored higher for four of eight individual HCAHPS measures than non-VA hospitals and lower for the other four measures. A second, small study found comparable surgical patient experiences in 2018 in VA and other hospitals in three cities, however.
“Ours is the only study of which we are aware that compares VA and non-VA patient experiences during the stress associated with the COVID-19 pandemic,” the authors asserted. “Our analysis is limited in that it only considers average VA and non-VA performance; there is substantial heterogeneity of hospitals within these two categories in terms of payer mix, location, and bed size, each of which is associated with HCAHPS performance.”
The researchers pointed out that their results differ somewhat from those comparing veterans’ outpatient care experiences at VA facilities and in community settings, explaining, “In the outpatient setting in 2016, veterans’ experiences in VA facilities were better than veterans’ experiences in community settings for communication, coordination, and provider rating but not for access in 2016; in addition, patient experience scores for all VA patients improved slightly from 2016 through 2017, but the gap between VA facilities and community settings did not change. In contrast, our baseline inpatient findings for 2017 showed higher ratings for non-VA care. In addition, our study can explore data from 2021 to show that VA care improved while non-VA care declined during the COVID-19 pandemic, with the VA surpassing other hospitals overall. Differences in setting, patient populations, and timing between our study and the earlier outpatient study make it difficult to know why the results differed.”
A possible answer is that several changes occurred within the VA healthcare system following the 2014 waitlist crisis:
The authors listed the following:
- VA patient care culture shifted, resulting in the establishment of a Veterans Experience Office that reports directly to the VA secretary,
- the designation of patient experiences officers in every facility, the development of performance plans inclusive of patient experience goals, and
- the identification of best practices and key drivers of good patient experience.
“Best practices were developed into toolkits to facilitate easy adoption at all VA sites,” the authors noted. “To the extent that quality improvement efforts resulted in more uniform care, Black patients and those in poor health, patient groups who are often underserved, may have benefited especially.
In addition, they wrote, the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act was implemented in 2019 to expand access and provider choice for VA patients by broadening eligibility for VA-paid community care from that in the 2014 Choice and Accountability Act.
“This shifted some VA patients to non-VA providers and was associated with reductions in VA hospitalization volume and an increase in VA-funded community hospitalizations,” the authors explained.
The study team said the analysis was limited because they had no information about patient rurality, which is associated with VA outpatient-care experiences and with general hospital patient experiences.
The researchers called for future research to assess whether the improved patient experiences in VA hospitals are sustained post-pandemic, what changes in care processes (such as patient-to-staff ratios), or unmeasured patient-mix characteristics (such as patient acuity) might have differed in community hospitals and VA hospitals, and whether the quality improvement strategies differed in nature and effectiveness.
“If effective and transferable strategies are identified, they could be disseminated to improve patient experience for non-VA hospitals,” the authors suggested.
Current rules allow VHA patients who live more than a 30-minute drive on average from the nearest VA facility to access the community care network for primary care, mental health and some extended care. For specialized care, veterans must live more than a one-hour drive from the nearest VA facility. Veterans also can use private care when a close VA facility does not provide the service they need or when their VA doctor recommends it.
In his bill, Bost is attempting to expand extended care options in the private sector and disallow the VA from considering telehealth availability when calculating community care eligibility. Another requirement would be consideration of veterans’ preference of where to seek treatment. Among other measures, the bill would create a 3-year pilot allowing patients to enroll in non-VA outpatient mental health or substance-use treatment without requiring a VA referral.
- Elliott MN, Beckett MK, W Cohea C, Lehrman WG, Goldstein E, Schaefer JH, Giordano LA, Saliba D. Inpatient Care Experiences Differ for VA and Non-VA Hospitals, With Different Patterns by Health, Race, and Ethnicity. Med Care Res Rev. 2024 Dec 5:10775587241300645. doi: 10.1177/10775587241300645. Epub ahead of print. PMID: 39636048.