HOUSTON — Lack of knowledge of the potential risks of antibiotic use was associated with increased expectations of being prescribed one, according to a new study, which said the lack of awareness is especially great among patients going to public health clinics.
The best answer, according to researchers from Baylor College of Medicine and the Michael E. DeBakey Veterans Affairs Medical Center, both in Houston, is for healthcare professionals to make a point of educating patients on what conditions can be successfully treated by antibiotics and the drugs’ downsides.
That might be easier for providers to refuse to prescribe them for common symptoms, they advised.
Their study in Annals of Family Medicine pointed out, “Patient expectations of receiving antibiotics for common symptoms can trigger unnecessary use.”1
The study team conducted a survey between January 2020 and June 2021 of 564 patients in public and private primary care clinics in Texas. The goal was to study the prevalence and predictors of patients’ antibiotic expectations for common symptoms/illnesses.
The study examined the (1) prevalence of patient antibiotic expectations for acute diarrhea, sore throat, cold/flu, sinus infection and bronchitis symptoms/illnesses, (2) differences in the prevalence of patient antibiotic expectations between primary care patients in a public and private healthcare system, and (3) predictors of patients’ antibiotic expectations for each symptom/illness.
“We surveyed Black patients (33%) and Hispanic/Latin patients (47%), and over 93% expected to receive an antibiotic for at least 1 of the 5 pre-defined symptoms/illnesses,” the researchers reported. They added that public clinic patients were nearly twice as likely to expect antibiotics for sore throat, diarrhea and cold/flu than private clinic patients.
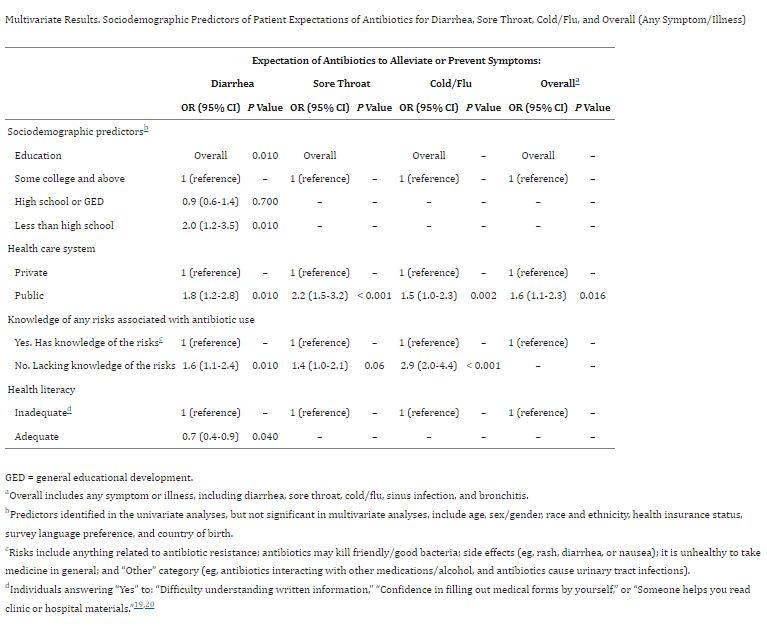
“Lack of knowledge of potential risks of antibiotic use was associated with increased antibiotic expectations for diarrhea (odds ratio [OR] = 1.6; 95% CI, 1.1-2.4) and cold/flu symptoms (OR = 2.9; 95% CI, 2.0-4.4),” the researchers explained. “Lower education and inadequate health literacy were predictors of antibiotic expectations for diarrhea. Future antibiotic stewardship interventions should tailor patient education materials to include information on antibiotic risks and guidance on appropriate antibiotic indications.”
Background information in the article advised that patients often receive antibiotic prescriptions to treat common viral symptoms/illnesses, such as respiratory tract infection, cold/flu and diarrhea, despite guidelines recommending against these practices.
“Individuals’ knowledge, beliefs and expectations may contribute to inappropriate antibiotic use,” the report noted. “These prior studies, however, did not examine the independent effects of knowledge of antibiotic risks and sociodemographic factors on patient expectations of antibiotics for common symptoms/illnesses.”
Patient Education is an Issue
The authors concluded that differences in patient education, knowledge of harms/risks, health literacy and the healthcare system itself can foster inappropriate patient expectations of antibiotics for common symptoms.
The study recommended that future stewardship interventions to reduce inappropriate patient antibiotic expectations should inform patients of the symptoms/illnesses that antibiotics treat and emphasize the individual harms/risks of antibiotics to themselves or those close to them.
Of those surveyed, about 84% believed that antibiotics would improve bronchitis, followed by sinus infections (72%), sore throat (66%), cold/flu (64%) and diarrhea (36%). Compared with private, public clinic patients were nearly twice as likely to expect antibiotics for diarrhea (odds ratio [OR] = 1.8; 95% CI, 1.2-2.8; P = 0.009), sore throat (OR = 2.2; 95% CI, 1.5-3.2; P <0.001), cold/flu (OR =1.5; 95% CI, 1.0-2.3; P = 0.002) and overall (OR = 1.6; 95% CI, 1.1-2.3; P <0.016).
“Educational level predicted patient antibiotic expectations for diarrhea, with patients with less than a high school education expecting antibiotics 2 times more than college-educated patients (95% CI, 1.2-3.5; P = 0.01),” the researchers wrote. “Additionally, patients with adequate health literacy were 30% less likely to expect antibiotics to help treat diarrhea (P = 0.04). Sex, race/ethnicity, health insurance, survey language, and country of birth were not significantly associated with patient antibiotic expectations for these symptoms.”
Overall, 37% of patients apparently lacked knowledge of antibiotic risks, with the proportion of patients with knowledge of antibiotic resistance higher in private compared with public clinic patients. In addition, the proportion of patients with knowledge of antibiotic side effects was lower in private vs. public clinic patients.
“Lack of knowledge about antibiotic risk(s) was significantly associated with increased antibiotic expectations for diarrhea (OR = 1.6; 95% CI, 1.1-2.4; P = 0.01) and cold/flu symptoms (OR = 2.9; 95% CI, 2-4.4; P <0.001) and was marginally associated with sore throat symptoms (P = 0.06),” according to the report.
The good news, according to the authors, is that other studies have shown that “patients with high antibiotic expectations and limited knowledge of risks also expressed trust in clinical advice, including willingness to consider alternative/non-antibiotic treatment options if counseled appropriately and involved in shared decision-making. In addition, patient-clinician counseling on patient-level adverse outcomes (eg, C. difficile infection and severe drug interactions/complications) may be more impactful than discussing societal harms or antibiotic resistance.”
- Laytner LA, Trautner BW, Nash S, Zoorob R, et. Al. Lack of Knowledge of Antibiotic Risks Contributes to Primary Care Patients’ Expectations of Antibiotics for Common Symptoms. Ann Fam Med. 2024 Sep-Oct;22(5):421-425. doi: 10.1370/afm.3161. PMID: 39313338; PMCID: PMC11419724.